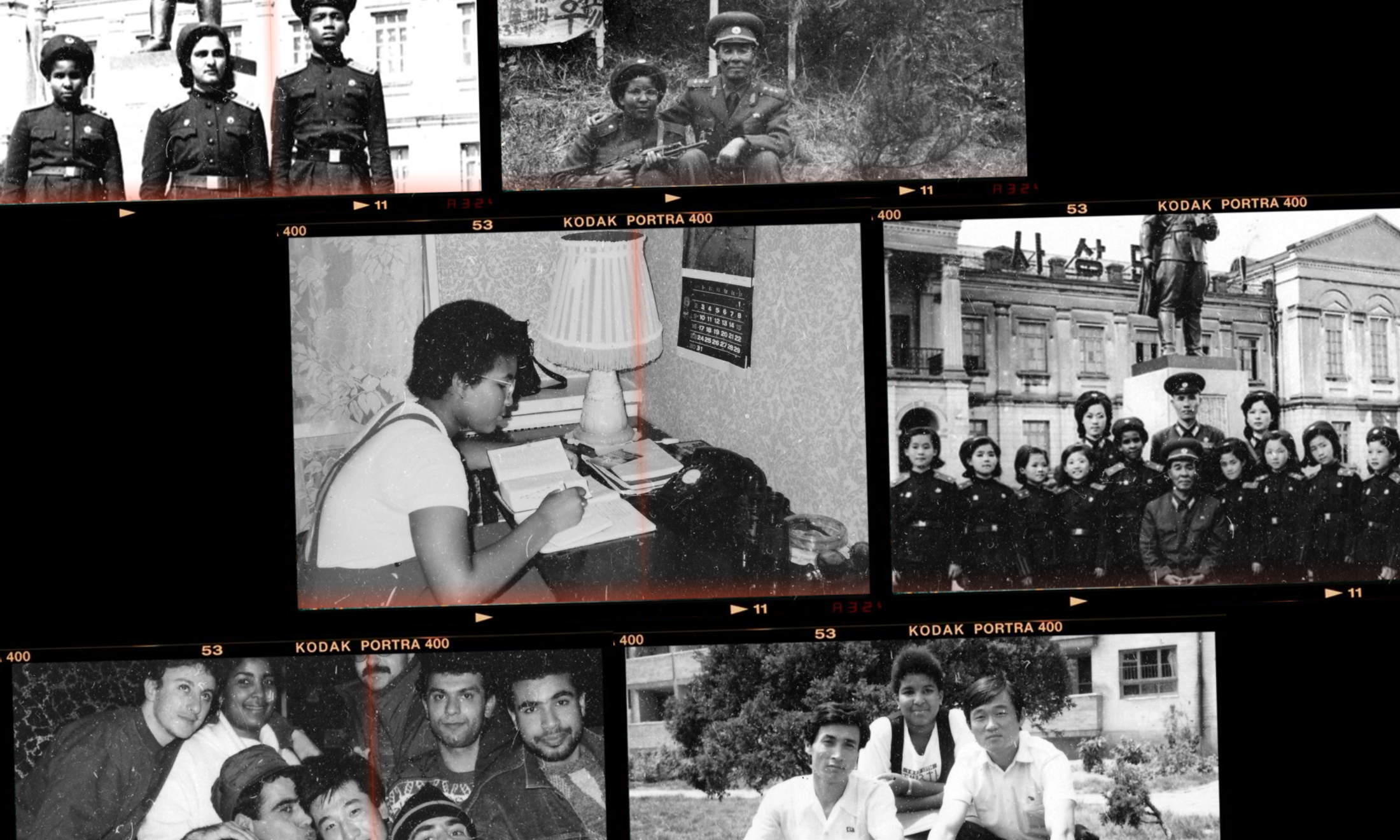
Black women are neglected by HIV-prevention services, but we need access to PrEP
Daniella de Block Golding
18 Sep 2019
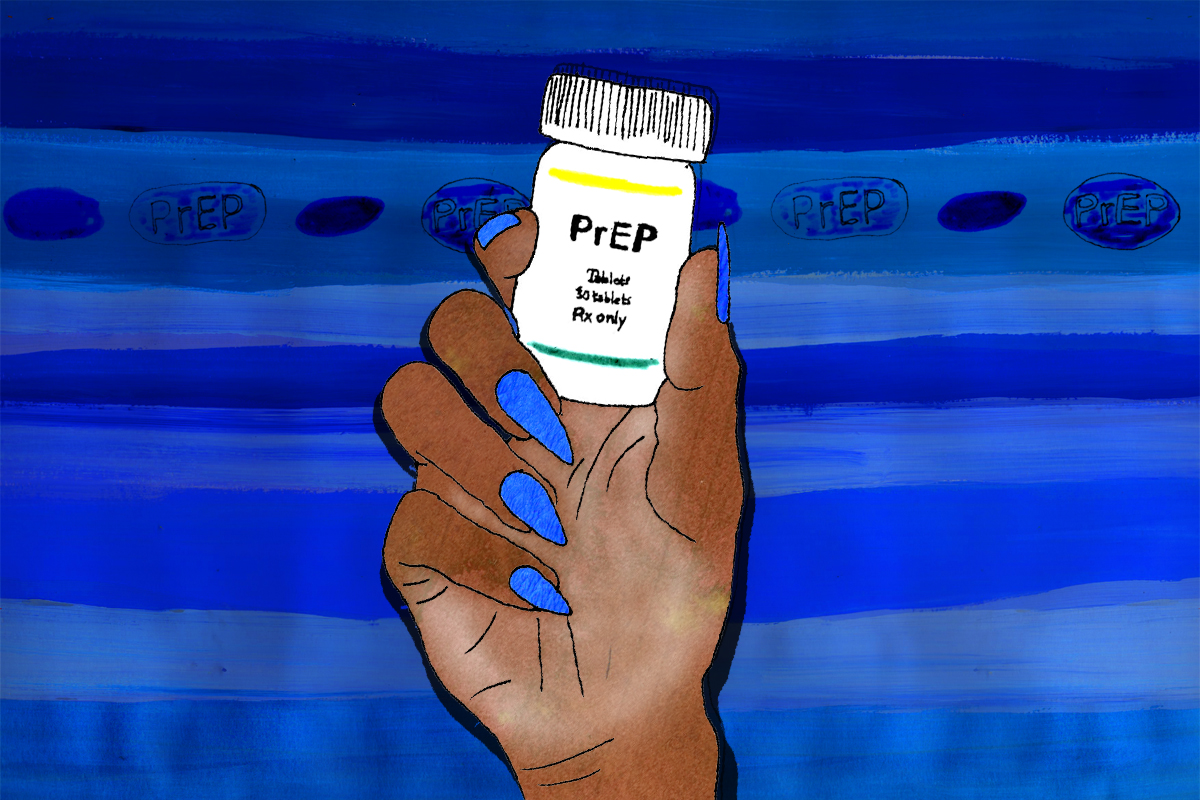
Illustration by Tessie Orange-Turner
When mainstream media talk about PrEP and HIV, they talk through the voices of cis white gay men or the medical community, often through throwing around statistics on the prevalence of HIV in sub-Saharan Africa. These perspectives are all key parts of the discussion, but where are the voices and experiences of black people, and in particular, women and queer folk of colour?
Despite the fact that communities of colour are recognised as being at a higher risk of HIV and other STIs compared to other demographics, we are being left behind in terms of improvements in our sexual health and sexual health care. Public Health England data shows that people of colour continue to experience disproportionately high rates of STIs and HIV for a whole host of reasons, and studies from clinics in both the North West and South East of the country show that we have much lower attendances to sexual health clinics. Services are not working for us and we need to look at why.
What is PrEP and who can take it?
One of the clearest examples of the healthcare gap is evident in access to PrEP, an oral medication which is taken to reduce the risk of HIV transmission. PrEP has been FDA approved since 2012 but has only been used by the NHS in England since 2018, and even then it is only being incorporated at present as part of a feasibility study known as the IMPACT trial. PrEP is thought to be up to 98% effective if taken correctly, and side effects are minimal. It can be taken by any gender, both cis and trans, and can protect against HIV transmission via anal, vaginal and oral sex. PrEP has been associated with reducing HIV transmission amongst men who sleep with men (MSMs) in London between 2015-2017 by over a third.
Approximately 13,000 people in England are now taking PrEP as a part of the IMPACT trial (which is looking at how services around PrEP should be implemented, rather than whether the medication works), and vastly more are using it through internet sales. Whilst this is all fantastic news, there are concerns that the trial is currently too narrow in scope: early reviews suggest that around 4% of those included in the trial are not men who have sex with men. In other words, only 4% of trial participants are cis or trans women. This is a problem as over a third of people accessing HIV services are women. There is a disconnect between the numbers of women at risk of contracting HIV and the numbers of women accessing PrEP. This is particularly concerning for black women as we make up over two-thirds of women living with HIV in the UK.
A number of factors play into this inequality. “HIV mirrors the inequality that we see in the world,” explains Will Nutland, co-founder of Prepster, a volunteer-based organisation who aim to educate and agitate around PrEP. Will explains that the needs of women and people of colour around sexual health are being silenced through a lack of representation at the level of who is making and directing policy. There is also a generalised underfunding of sexual health provision and under-resourcing of some of the community organisations that may be best placed to do this work. For some women and people of colour, there are also ongoing difficulties of competing life priorities and practical considerations such as costs around accessing clinics, booking an appointment or attending with children.
Is public messaging around sexual health speaking to people of colour?
Women and communities of colour are sometimes described as “hard to reach” or “difficult to engage” by the medical establishment. This belies the reality that there are successful outreach models which demonstrate that if you make an effort to provide outreach in strategic locations and appropriate and culturally competent ways, you can easily engage these key groups. “They’re not hard to reach, they’re just not invested in enough,” explains Will. Research shows time and again that communities of colour are asking for sexual health education and services through broader means than just the sexual health clinic – be it from face-to-face outreach, school education, social media or more mainstream advertising. This does mean, however, providing funding for organisations outside of traditional sexual health spheres and recognising the nuances of this delivery, such as who is delivering the information and how?
In the case of PrEP, we know that many of the clinics that are included in the PrEP IMPACT trial (the only way to get PrEP on the NHS currently) are not spaces where women of colour would be accessing sexual health and contraceptive support. Around 47% of women get contraception and sexual health care from their GPs, so why are GPs not being included as sites for PrEP initiation?
The current guidelines on PrEP for women are also vague; they state that women “may be considered for PrEP” if they are at increased risk through a “combination of factors”. It isn’t clear how many of these factors should make both the woman or the clinician start thinking about PrEP and means that a woman’s access to PrEP is very dependent on the interpretation of the guideline by the clinician that they see that day. Other countries take a much more patient-led approach to PrEP for women; for example in South Africa healthcare providers have taken the view that if someone is asking for PrEP, it is because they deem themselves to be high risk. A patient may not disclose their risk fully, and so if they are asking for treatment this is considered a sufficient indicator of need.
What can be done to improve PrEP access for patients of colour?
In the UK, we are seeing action to include communities of colour and women in the conversation around PrEP, and sexual health more generally. Organisations such as Prepster, who educate and agitate for PrEP access, and NAZ, who aim to provide HIV and sexual health services for men and women from black and ethnic minority backgrounds, are working to improve the visibility of people of colour around sexual health and to provide support and services. There are also initiatives funded by the Public Health England Innovation fund such as MobPrESH (mobilising in PrEP and sexual health), Sholay Love, which specifically caters to South Asian Men who have sex with men, PrEP and Prejudice and PrEP Champions, a partnership project. There is an ongoing acknowledgement of the issue in the Health and Social Care Committee report 2017-19.
MobPrESH, run by Prepster, trains women across Bristol, London and North Yorkshire to become peer mobilisers who can act as educators, advocators and supporters for women in their communities around PrEP and sexual health issues. Josina Calliste, a project coordinator for MobPrESH, highlights the need for the project to be run alongside reproductive justice frameworks which recognise the intersecting oppressions that prevent people from accessing their reproductive rights. MobPrESH has created peer-led approaches and opportunities for women to discuss sexual health issues through events such as cooking evenings, supper clubs, coffee mornings, hairdressers outreach as well as running workshops and attending carnivals and pride events.
“We need to be talking about sex and relationships in general, to allow women to tease out their needs in relation to better and healthier sex,” explains Josina, going on to describe the need for conversations about PrEP with women to be framed differently. Talking of how women are assessed around the need to start PrEP, she says, “You can’t just walk up to a woman and ask her if she’s ever had a rectal STI, you know?!” Asking interrogative and deeply personal questions around medical history and sexual practices are not the most strategic ways to invite women to open up and start thinking about their sexual health. This instead needs to be provided via a more personalised and collaborative approach.
Women and people of colour being on the peripheries of PrEP is a global issue
The lack of representation of women and queer communities of colour using PrEP and sexual health clinics generally is mirrored globally, and we are seeing other countries also taking steps to provide a much more tailored and community-led approach. San Francisco Department of Public Health (SF DPH) for example, are using peer navigators to help create a community-led network for people of colour and women taking PrEP. The SF DPH are also using alternative providers such as primary care physicians and local pharmacies to initiate PrEP rather than asking people to cross town to use services. They are taking steps to improve community awareness by using targeted information campaigns at key events such as black women’s networking events, basketball games and at black hairdressers and bars. They have also done extensive research amongst target audiences to ensure that social media campaigns are hitting the right notes after first attempts were deemed fetishising and overly sexualised.
Organisations in South Africa are also using youth navigators to help support people in taking PrEP. They are using technologies such as WhatsApp to provide direct lines for clinical advice, and are creating WhatsApp groups for rural PrEP users to maintain contact with others using the medication. They have found that the inclusion of PrEP storylines in popular soap operas and the use of relevant celebrities as PrEP ambassadors has also increased the understanding and support of PrEP amongst communities of colour.
We need to continue to support each other in improving our sexual health and reducing our risk of contracting HIV, but health services need to support us to do that by recognising that there is a gap in terms of the reach of many interventions around HIV and improvements in sexual health. That means continuing and increasing funding for community-led groups and recognising the need to target different social groups with specialised strategies and approaches.
Thinking of her dream list for what services could look like, Josina describes “long-term funding cycles for projects that work; building sexual health services into facilities that black women already use; building tailor-made services for women of colour; and ensuring cultural competence in all that we do”.
We are moving into an era where NHS directors are going to be faced with even starker choices about what our health system funds. The temptation will be to support headline-worthy high tech options, but we need to remember that much of reducing health inequality, particularly in the sexual health sphere, lies in elevating the voices of and responding to those who may be most affected but may not be shouting the loudest.
This article is part of gal-dem’s Sexual Health Awareness Week series. You can keep up with the series here