
In March I received an offer from King’s College London to study an MSc in Affective Disorders. This includes the study of disorders such as major depressive disorder and anxiety disorder. No more than one second after reading my acceptance letter did I begin to panic about funding – how the hell was I going to pay for it?
Nothing assured me more of the fact that I want to train as a clinical psychologist than the responses I received after launching my crowdfunding project, #BackBossy, to raise the funds for my masters course. Not only were people aware of the lack of research being done on adolescent mental health, particularly within the BME community, but people were also coming forward with their own experiences of mental health issues.
The fact is, when you are an adolescent (or in early adulthood), you are at higher risk of developing a mental health disorder. There are a variety of proposed explanations from scientific research but no one really knows why individuals in this age group are more susceptible to psychological disorders. Scientific research has not been able to put forward a concrete or coherent explanation. However, several risk factors such as family history, early life experience, a history of abuse and socioeconomic environment have been identified.
The representation of mental health disorders among the adolescent population is finally getting the attention it deserves: conversations around depression, social anxiety disorder, schizophrenia and bipolar disorder are taking place and the stigma appears to be reducing. But when I imagine someone with depression, I don’t picture someone who looks like me. Even when I myself have personally suffered with the disorder, and know many other black women who have too.
Very few people are talking about this issue within the black community. This is not because we don’t suffer with mental illness. Black people are positioned within society in such a way that mental health issues are arguably inherent: being continually disenfranchised and oppressed by society, told you are not smart, not beautiful, and — in extreme cases of racism — not human, it is reasonable to assume that this is will affect you on a psychological level. I think the issue is that the way psychological disorders are studied and modelled do not reflect the cultural values held in black communities. For example, I know that in Nigeria, where my parents are from, religion and spirits are held highly when talking about one’s own psychological well being – such factors are not considered in our Western models of mental health.
Within the black British community, mental health issues are experienced differently. First generation migrants who had to integrate into British culture whilst being victims of visceral racial abuse and discrimination will have faced a different kind of psychological trauma compared to second and third generation migrants, who face fights with implicit racism, white curriculums and Eurocentric standards of beauty.
This is not helped by the fact that the majority of healthcare professionals who work in therapy or in treating mental health are white. As a psychology student I have so many issues with how research and treatment of affective disorders is carried out in the UK. When the efficacy of a new treatment is being trialled, the sample individuals are usually from a white and middle class background. Race is never brought into the topic of mental health.
This then has effects on the number of clinical psychologists available from ethnic minority backgrounds. For example, in the 2014 entry of clinical psychologists trained on an NHS funded course, out of the 578 accepted, 3% were Asian and only 2% were black. An important part of providing better mental health services for BME individuals is making sure that a patient can access help from a professional of their ethnic group, if they prefer. Being able to talk to someone who looks like you and understands your cultural experience is important to some individuals. While others may want to be treated by someone who they cannot relate to, the point is that they are given the choice.
Why is there a lack of BME clinical psychologists? One of the barriers that I am personally facing is funding. How is someone from my background expected to progress in this increasingly privatised and commercialised educational system if there are no means of support? I’m part of the £9,000 per year tuition fee-paying cohort of undergraduates. With the government replacing maintenance grants with loans, and increasing the cost of tuition, I’m glad to be in the final year of my psychology degree. Yet I am about to be expelled into the brutal, unsupported abyss of postgraduate studies. Coming from a low-income, single-parent family, I am not a position to raise the £20k+ it will cost to undertake a masters. Despite several scholarship applications, part-time employment, and the new government postgraduate loan, there is still a shortfall in my budget – hence the launch of my crowdfunding project, #BackBossy.
I am interested in how social adversity impacts the diagnosis, treatment and management of affective disorders such as depression and anxiety. In the future, I want to train to be a clinical psychologist and help those suffering with affective disorders from low socioeconomic and ethnic minority backgrounds like myself.
I want to work specifically work with black British women, in order to reveal their hardships during diagnosis and treatment. A recent article in Media Diversified by Guilaine Kinouani described this plight perfectly: “I, as a Black woman, I’m more likely to be prescribed psychotropic medication than to be offered therapy…my chances of being coerced into psychiatric ‘care’ if I’m in distress are still much higher than average; and I’m less likely to want to engage with mental health services.” These are the issues that keep me up at night. I’m tired of meeting incredible black women who are suffering with mental health issues, but aren’t being offered the services that meet their needs.
I’m tired of coming across statistics like “African Caribbean people are five times more likely to be diagnosed with schizophrenia” or “Black people are 50% more likely to be detained under the Mental Health Act via police referrals, restrained and forced to take medication” . Finally, I’m tired of reading journal articles on the study of major depressive disorder that use an all white sample.
A master’s degree that furthers my understanding of affective disorders will not fix the social inequalities that our current mental health services face, and it is futile to approach it from solely a scientific perspective. Raising awareness and addressing the challenges in the services available is critical and I hope my crowdfunding project, #BackBossy, is helping to do that.
I am fully aware of the fact that a black woman carrying a nickname like “bossy” is racialised… but that’s a discussion for another day. Today, I’m trying to get this black body into the white space of mental health research.

Britain’s policing was built on racism. Abolition is unavoidable

Against the binary: imagining a future of holding my chest high
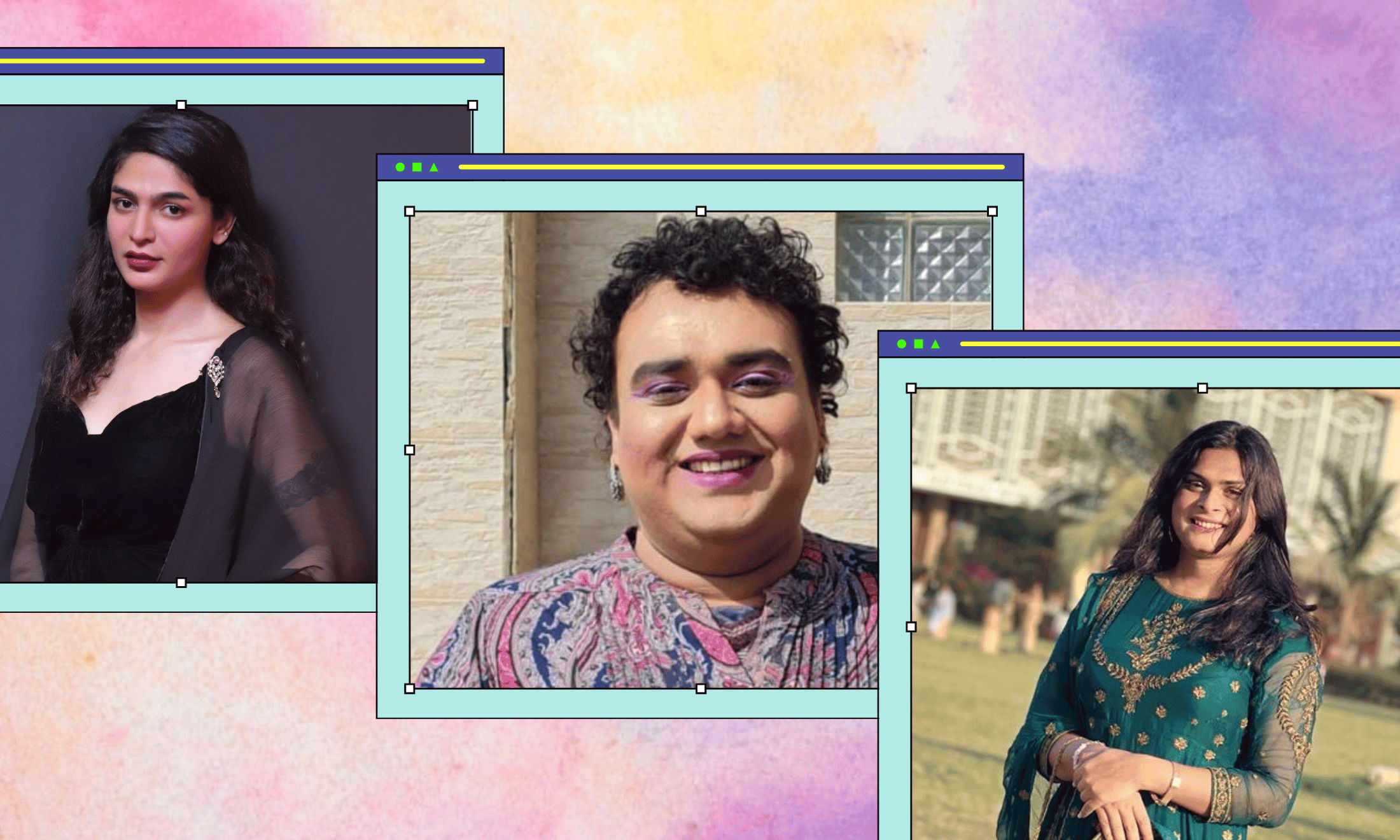
How Pakistan’s Khwaja Sira and transgender communities are fearing and fighting for their futures






