Illustration by Charity Atukunda
Death wasn’t supposed to be in the job description for ethnic minority key workers
The pandemic was a ticking time bomb that was always going to hurt key workers from black, Asian and other ethnic minority backgrounds disproportionately. Nimo Omer speaks to the workers whose lives have been put in danger.
Nimo Omer
27 Apr 2020
Many of us move blissfully unaware through life without asking any questions. Where does this come from? How did my package get here so quick? Who delivered this food to my doorstep? Are they okay? We blindly trust that these things will take care of themselves, or perhaps we are wilfully ignorant, safe in the knowledge that we will never really have to confront any of it. Covid-19 has removed these moments of regularity and turned our entire world upside down. The system that has always been invisibly held together by things we don’t understand or think about is crumbling before our very eyes.
Coronavirus has exposed the glaring reality that we live in a fundamentally unequal society. Alongside the unprecedented death toll and financial strain, the pandemic has shone a harsh light onto the working conditions of our key workers from black, Asian and other immigrant and ethnic minority backgrounds. While many of those people – the healthcare professionals, the care workers, the bus drivers, the cleaners – have been telling us of the problems that they face for some time, it is only now, in a time of extreme crisis, that we have begun to listen. And while the response of the nation has been one of overwhelming gratitude and appreciation, thanks to the whitewashing of the media, it has largely missed those putting themselves at the greatest risk.
New data from NHS England has revealed that more than 16% of coronavirus victims in England were BAME people. A Guardian analysis has found that of the 53 NHS staff known to have died in the pandemic thus far 68% were BAME. Another study from the Intensive Care National Audit and Research Centre showed that BAME patients made up 33.6% of those who have contracted the virus, despite only making up 14% of the population. The government has recently opened an inquiry into the disproportionate impact of coronavirus on BAME communities after significant pressure from the British Medical Association, but no information has been released about the timeframe and what kind of data would be shared.
We must not forget that in these numbers and statistics lie the human stories of very real, complex, people across the country. People like 36-year-old mother of three Kayla Williams, a black woman living in south London, who died in her flat after having called 999 with severe coronavirus symptoms. She was told she was “not priority”. Or Mary Agyeiwaa Agyapong, a 28-year-old pregnant nurse who had worked for five years at Luton and Dunstable University Hospital. Her baby survived but Mary passed away on 12 April, two days after being admitted to hospital.
And so the question needs to be asked, why is this happening?
“Don’t send me on a suicide mission”
There are a large number of people of colour working in healthcare in this country, reflected by the reality that the first four doctors who died from coronavirus were all Muslim immigrants with roots in Africa and South Asia. Alongside the fact that 44% of medical staff who work for the NHS are ethnic minorities, figures from the General Medical Council show that in 2018 53% of those who joined the medical register came from outside the country to do so – a rise from 39% in 2015. Analysis of NHS data by the Royal College of Nursing has also shown that nurses from BAME backgrounds form the majority of nursing staff in London, where the largest number of coronavirus cases have been reported.
But in addition to the high levels of staffing, BAME healthcare workers have their own theories on why they are dying at disproportionate rates. Maryam* is a junior doctor currently dealing with coronavirus patients on a regular basis. “It’s just another one of those things where black and brown bodies are seen as expendable,” she says.
There are claims that BAME staff are being chosen to work on coronavirus wards more frequently than their white counterparts. In an interview with Nursing Times, Carol Cooper, head of equality, diversity and human rights at Birmingham Community Healthcare NHS Trust, said that “BME staff feel that they are being put on Covid wards and exposed to patients with Covid over and above their colleagues.” She also said that BME staff “feel that there is a bias – the same bias that existed before they are feeling is now influencing their being appointed and they are terrified, everybody is terrified”.
For other BAME staff members, it is the widely reported lack of personal protective equipment (PPE) and testing that is leaving them feeling unsafe. Dr Maryam says that healthcare workers on her ward were being given PPE that expired almost four months ago and an orthopaedic nurse, Nigella*, who works in University Hospital Coventry and Warwickshire, reveals that her hospital has had to reuse masks. “They’re not meant to be reused, but now they’re telling us we have to clean the mask with tristel solution and reuse it when we interact with other patients,” she explains. “This is a compromise on healthcare. The fundamentals of healthcare is not to reuse anything, we don’t reuse needles, do we?” She concludes with a sentiment echoed by Dr Maryam and healthcare professionals across the country: “At least protect me so I can do the best job I can do, don’t send me on a suicide mission.”
Aisha*, a nurse who works in an emergency and acute medical care ward in Coventry and has been self-isolating after showing symptoms, also expresses that she feels profoundly unprotected. “We haven’t been tested. I’ve been ill for over a week and they’re still not going to test me. Many of the staff might be spreading it amongst each other and to the patients but they don’t know because they’re not testing anybody.” After a short pause, Aisha adds, “Every day I pray to God that my kids don’t get it.”
Some BAME families (Indian, Pakistani and British African) are more likely to live in intergenerational households and Robin, an artist and Masters student in law and business, caught coronavirus from their grandmother Deborah*, a carer at a nursing home. “When you have it you can’t do anything,” she says. “I was just laying in silence. The whole house was just silence. You can’t even watch TV. It’s too much energy to even open your eyes… I was really, really ill for three days but the days before and after even though I was still ill, like really ill, it wasn’t to the point where I couldn’t do anything. The rest of the time I was alright. But regardless of that I still had to cook and clean because I had to take care of my nan. It was a lot.”
Regardless of how severe her symptoms were, Deborah’s place of work would frequently call to ask when she was coming back in to work. “They said she has to email in. How the hell can she email in, she can’t even sit up? They said she has to fill something out on the NHS website like a corona slip and email it to her manager, all this shit. And I was like she can’t do that and I’m still ill, I can’t do that, so I told them I’ll send it whenever I feel like and don’t call back here. That’s literally what I said.” Robin’s frustration is palpable. Taking a long breath she adds that her grandmother is “not even the type of person to call in sick” and that how they’re acting is “mad”. Her nan is not alone in this – The Independent revealed that numerous care homes are refusing to give sick pay to workers who’ve been told by the government to stay at home during the pandemic.
In all of this discourse, that seeks to valorise and heroise key workers like doctors, nurses and carers, there is a profound truth that is missing. That they too have families, that they are scared, and that ultimately they have never consented to putting themselves in such a precarious and dangerous situation. The proliferation of war-time rhetoric has moved the discourse around coronavirus, and in turn, the measures to mitigate its damage, to profoundly unhelpful places especially once we consider who is on the “frontline”.
Dr Maryam says that “the whole war-like language really upsets and triggers me because it makes me feel like I’ve been conscripted. No healthcare professional signed up to risk their lives”. She goes on: “With any other infectious disease there is equipment we’re supposed to wear, there are vaccines that we’re supposed to get, tests are supposed to happen regularly. So the whole idea of healthcare professionals putting their lives on the line because it’s a part of our job description is bullshit.”
By this point, many minority healthcare workers have lost their lives helping this country in the best way they knew how – through medicine – in a society that has done nothing but peddle anti-immigrant rhetoric and stoke racist fears. But it is only now, when these stories are completely unavoidable and overwhelming, and when lives are lost, that people are claiming to finally see the benefits of having us here.
“There isn’t a genetic predisposition to the disease at all”
Coronavirus became a racialised disease from the moment it was first reported and racism spiked against East Asians, while fake news was spread that melanin could protect black people against coronavirus. But there is limited evidence that being from an ethnic minority background should inherently leave you more or less vulnerable to coronavirus for biological reasons.
Dr Elisa Pierie, a social scientist and expert in pandemic preparedness, stresses that current evidence “doesn’t at all suggest a genetic predisposition or a particular susceptibility to the disease”. Instead, she looks to socioeconomic reasoning. “If you’re looking at cleaners and less professionalised medical health jobs, they are filled with people who are of BME origin,” says Dr Elisa. “In that sense, it might be more reflective of injustices or unequal division of labour in society and the fact that the NHS is underfunded. We can also link it to nutrition, poverty, income disposal.”
Dr Elisa also highlights the importance of understanding that pandemics affect groups differently. “The measures that are put in place therefore will have different impacts on people too,” she says. “Like any other crisis they are likely to exacerbate inequalities and make life much harder for certain groups of people who are already experiencing marginalisation or are deprived in other ways”.
It is within this context that we need to carefully look at the way Covid-19 is disproportionately impacting our communities. Yvonne Field, the founder and CEO of African Diaspora social enterprise The Ubele Initiative, summarises it succinctly: “Coronavirus is not the great leveller. What it’s showing clearly is long-standing systemic entrenched institutional inequality. The system is designed, stacked, run, its roots are based, on inequality. We’re not even considered, let alone centred. It’s like we’re a whole big blind spot. And if we’re not a blind spot we’re an inconvenience.”
As new research from The Runnymede Trust not only suggests that Covid-19 is widening the wealth gap between BAME households and white Brits, but that “the effects could last for a generation”, the enterprise has begun a campaign for an independent public investigation into why BAME communities are being disproportionately infected by Covid-19, and is offering practical support to those communities during the crisis.
“They’ve been neglecting drivers’ welfare for years”
After a decade of austerity, with very few exceptions, many key workers have become underpaid invisible workers that often go ignored and unnoticed. Whilst in the context of coronavirus key workers has often been synonymous with healthcare worker, we must also acknowledge the cleaners, bin collectors, Uber drivers, warehouse operatives and bus drivers that are keeping our society functioning – despite often working in dangerous conditions for little pay and almost no recognition. In a similar vein we see that these occupations are disproportionately made up of BAME workers. For instance, in a report conducted by the Equality and Human Rights Commission up to 44% of cleaners in London, and 16% across England, are ethnic minorities.
Moe, who’s been a bus driver for 10 years, speaks about the ways in which TfL has been “neglecting the drivers’ welfare conditions” for years. He mentions how providing “toilets” and hygiene generally was never a priority for the bus companies, explaining how sometimes bus drivers had to go in the bushes and didn’t have access to basic necessities like soap.
“What this virus has done has exposed the failures of the capitalist system, it’s highlighted all the problems that the drivers day-to-day faced and what they never had,” he says. Bus drivers are also generally more vulnerable and are more likely to have underlying health conditions – 74% of the bus drivers that took part in a study conducted by Loughborough University were defined as being overweight or obese and at higher risk of heart disease due to “lengthy periods of sedentary behaviour”.
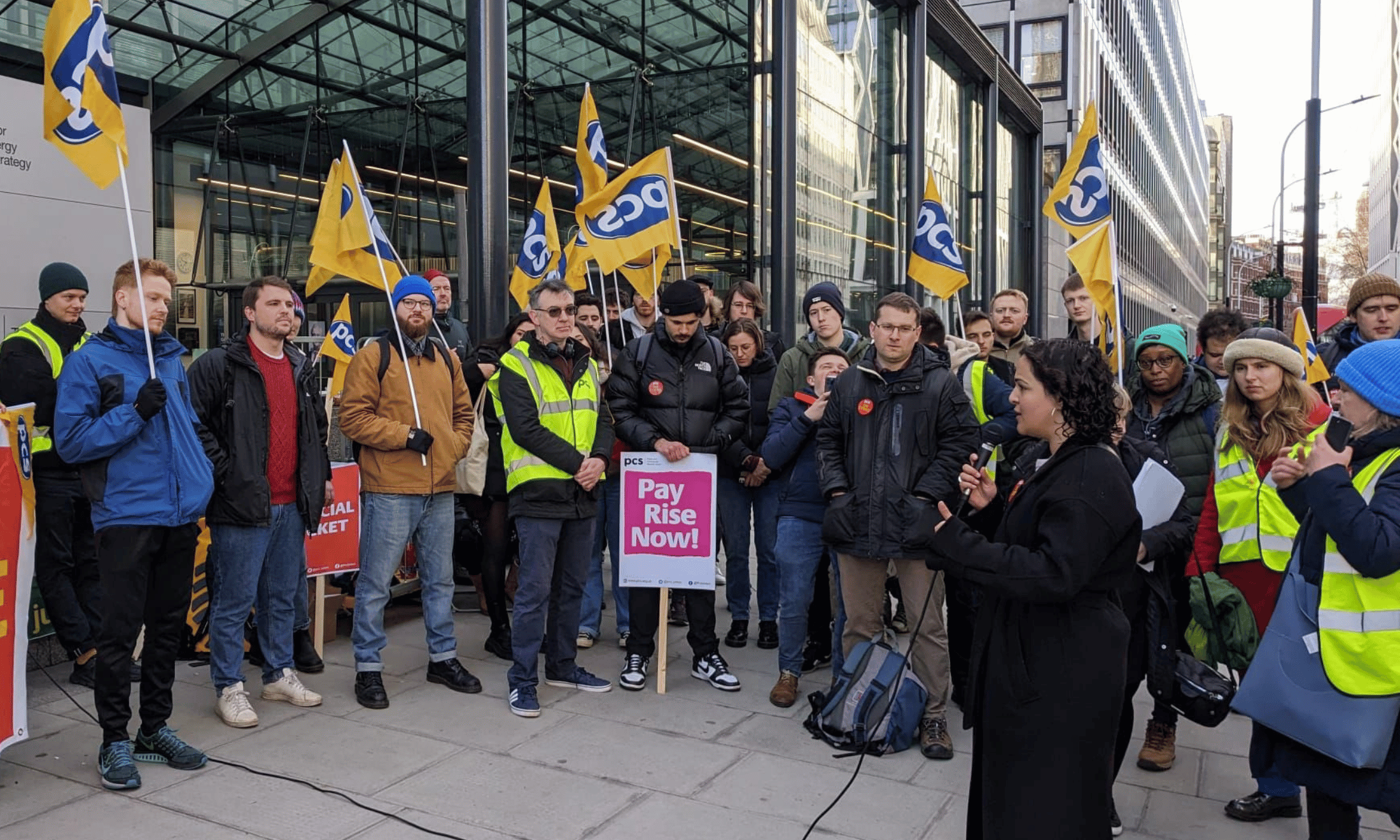
Unfortunately it’s been an uphill battle for bus drivers in London, and across the country, to secure basic rights even in the midst of a global pandemic but, as Moe points out, they were able to make some gains only after bus drivers began to pass away and “from the back of our trade union leaders who absolutely pressed for our voices to be heard”. As a result, hand sanitisers have been rolled out, perspex film has been fitted on the speaker holes of the bus drivers cab, antiviral cleaning and an enhanced cleaning regime in the cabs has been introduced.
Like many other key workers, Moe has a family waiting at home for him, a wife who is expecting and who at one point was showing symptoms. His colleagues have been passing away and he has developed severe anxiety. His job is undeniably arduous and incredibly important yet he says that he and his colleagues have felt “disposable”, like they are “just a number” and that “they can just replace us”. He paints a bleak picture of our bus system, one that needs to change.
“We’re not listened to and it needs to stop”
It has become increasingly clear that similar to other times of great distress, like natural disasters or economic crises, it is those who are at the bottom of society’s totem pole that suffer the most. Whether it is because we disproportionately represent frontline workers or because we are more likely to be living in poverty, working in precarious, low paid jobs, living in overcrowded accommodations and in food deserts, our vulnerability to this virus is glaringly obvious.
At a roundtable hosted by Labour leader Keir Starmer on 24 April, Baroness Doreen Lawrence, who is leading Labour’s review into the impact of coronavirus on BAME communities, expressed her concern and frustration. “We’re not listened to, we’re brushed aside and it needs to stop. Our people are dying,” she said. In her succinctness, we find the central issue. We are dying. In staggering numbers. And yet the pandemic has hurt us in ways that we probably don’t even realise yet. This is why the independent investigation that the Ubele Initiative is calling for is so crucial. There needs to be a reflection on this horrifying moment in time.
The exasperation, anger and at points despondency that was expressed by all those quoted in this article is not new, but many feel particularly disillusioned with the government’s response to Covid-19, from its initial glib and flippant reaction back in January and February to its fatal “herd immunity” strategy in March, to now. Over 150,000 confirmed cases and almost 21,000 deaths later. How many of those deaths were preventable? How many lives were unnecessarily cut short? We may never know. For now, we will have to try to find peace, learn to lean on one another and strive to hold those in power to account.
*Names have been changed to protect identities

Britain’s policing was built on racism. Abolition is unavoidable
How Pakistan’s Khwaja Sira and transgender communities are fearing and fighting for their futures

Their anti-rape performance went viral globally. Now what?