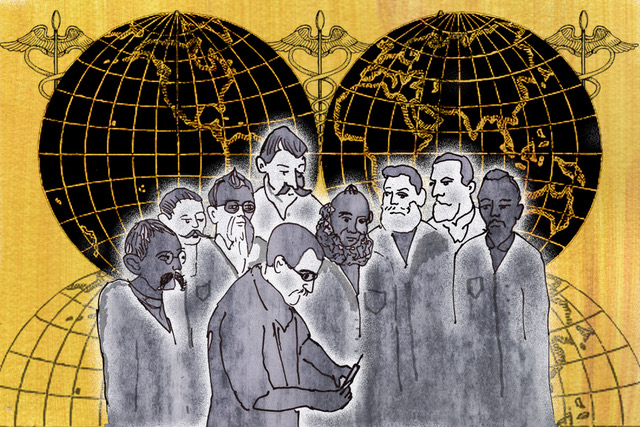
Illustration by Tessie Orange-Turner
Medicine has been so whitewashed that we’ve forgotten vaccination is a part of Black history
As a petition to ‘stop government plans to trial Covid-19 vaccines on Black people’ grows, it's worth remembering the story of African slave Onesmius, who helped bring smallpox inoculation to the US in the early 1700s.
Annabel Sowemimo
09 Jul 2020
Illustration by Tessie Orange-Turner
“If I can be provocative, shouldn’t we be doing this study in Africa, where there are no masks, no treatments, no resuscitation?” said Jean-Paul Mira, head of intensive care at Cochin Hospital in Paris, during a live TV debate in early April when discussing the potential for subsequent Covid-19 vaccination trials.
Much criticism followed with high profile such as footballer Didier Drogba tweeting that “Africa isn’t a testing lab” and actor John Boyega being even more direct and stating that “Africa isn’t a testing lab you pieces of shit.”
There has been a long history of suspicion amongst Black, Indigenous and other marginalised groups receiving vaccinations, especially in the context of public health programmes implemented by Western charities or in low resource settings. For example, a polio vaccination programme in Northern Nigeria failed after locals believed rumours that the vaccination was a plan by the West to make them infertile. Within my own family circle, I have heard people state, “we don’t know what is in those things” and “you should have as few vaccines as possible”.
A petition to “Stop government plans to ‘trial’ Covid-19 vaccines on Black and minority ethnic groups” currently has in excess of 45,000 signatories at the time of writing. Some of the concerns include that this vaccine is being created in a much shorter timeframe than other vaccines and that “BAME communities” are at risk of catching Covid-19 due to “worse healthcare conditions in the UK and substandard levels of care”. There are currently two vaccination trials ongoing in the UK, ran by Oxford University and Imperial University in London, and neither are targeting “BAME” groups. However, there have been discussions about the vaccine being made available to BAME populations and other at risk groups first.
“There are currently two vaccination trials ongoing in the UK and neither are targeting ‘BAME’ groups”
One argument that persistently rears its ugly head in these discussions is that having vaccinations are fundamentally “not African” and strictly a Western, white practice. This could not be further from the truth. Enter Onesmius – a slave of African descent who helped bring the idea of vaccination to Europe; minimising the impact of a smallpox outbreak in Boston in 1721. In 1706, Onesmius, a man of African descent, was “gifted” to Puritan minister Cotton Mather after being purchased for the sum of 40 and 50 pounds and was renamed Onesmius. Cotton, who was a prominent figure in the Salem Witch trials, vowed to make Onesmius a “servant of Christ” and went on to write an extensive essay on “the Christianisation of the negroes”.
In 1714, Cotton’s responded to a letter he read in the Royal Society of London about the practice of inoculation (the introduction of a microorganism into a host to create an immune response) practised amongst “the Turks and others at Constantinople” which gave them very “slight symptoms” but resulted in them not dying of smallpox. Cotton’s response referred to a practice his African slave, Onesmius, had also undergone:
“…Enquiring of my Negro man, Onesimus, who is a pretty intelligent fellow, whether he had ever had the smallpox, he answered, both yes and no; and then told me that he had undergone an operation, which had given him something of the smallpox and would forever preserve him from it; adding that it was often used among the Guramantese and whoever had the courage to use it was forever free of the fear of contagion. He described the operation to me, and showed me in his arm the scar which it had left upon him; and his description of it made it the same that afterwards I found related unto you by your Timonius.”
After the smallpox outbreak began in Boston in 1721, Cotton used this knowledge to advocate for the inoculation of the population and this spread to other colonies. There is irrefutable evidence that the practice of inoculation predates this and some of the earliest examples are in the regions which would now be modern-day China and India.
Edward Jenner is credited with the eradication of smallpox through the development of modern vaccination procedures yet, the existence of inoculation in other parts of the world proceeds this by likely two centuries and is not known by most people. Modern medicine has intermingled, learnt and borrowed from other cultures. This is a fact. Many of the medicines we use today are purified forms and compounds of plants discovered in the Amazon rainforest (and elsewhere) and were used by local populations for healing benefits for centuries prior. Without acknowledging the rich tapestry of how modern medicine has come to be; we risk exclusionary history being taken as fact and causing marginalised groups to reject valuable interventions on the basis that it is “not for them” and placing them at risk of further subjugation.
“Without acknowledging the rich tapestry of how modern medicine has come to be, we risk exclusionary history”
As scientists across the world strive to develop a Covid-19 vaccine, we should all be seeking to support these efforts and most importantly, ensure that those that may benefit have access to it. Whilst we must continue to scrutinise and explore the ethics of all medical trials, we must too examine who benefits from the end product. The first Declaration of Helsinki was established in 1964 by the World Medical Association to create a standard for international research trials, which ensures that there is voluntary and informed consent, subjects have access to post-trial treatment and there is good accessibility of the resulting tested medicine to the general population. However, this is not enforceable by any international laws and there has frequently been a failure to ensure the latter.
Over the last few months, we have seen many discussions about who and how a Covid-19 vaccination could be rolled out if we are lucky enough to find one. There are concerns that those living in low resource settings may be left out due to pharmaceutical deals that place profit over people. There are fears that within high-income settings, like the UK, those that have been disproportionately affected, including the most economically deprived migrant communities, will not gain access to the vaccination.
The World Health Organisation has been working diligently to ensure that as beneficial information is generated knowledge is pooled together, so that profit does not hinder global progress in eradicating this virus. Unfortunately, some key countries continue to be absent from the discussion table as demonstrated at the recent Global Vaccine Summit.

Britain’s policing was built on racism. Abolition is unavoidable
How Pakistan’s Khwaja Sira and transgender communities are fearing and fighting for their futures

Their anti-rape performance went viral globally. Now what?