Louis Galvez/Canva
The Prevent duty is criminalising Muslims who seek mental health care
The anti-terrorism programme is having devastating consequences for Muslims and minority communities seeking services.
Mashal Iftikhar
10 Aug 2022
A patient is nervously pacing up and down the corridor of the psychiatric ward where I am the on-call doctor that evening. He’s reciting Surah Baqarah under his breath, the title of the second chapter of the Qur’an.
“It’s Baqra Eid soon, it’s all about sacrifice,” I explain to the nurse, who looks at him suspiciously. “Honestly, I think he’s just missing his family and is sad to not be with them for Eid. I’m on night [shifts] over Eid and I’m feeling miserable about it too. We’re both feeling the sacrifice.”
Here I was with an NHS colleague, compressing centuries of Islamic philosophy on the meaning of sacrifice, so they wouldn’t be alarmed by a clearly distressed Muslim patient turning to his faith as source of comfort.
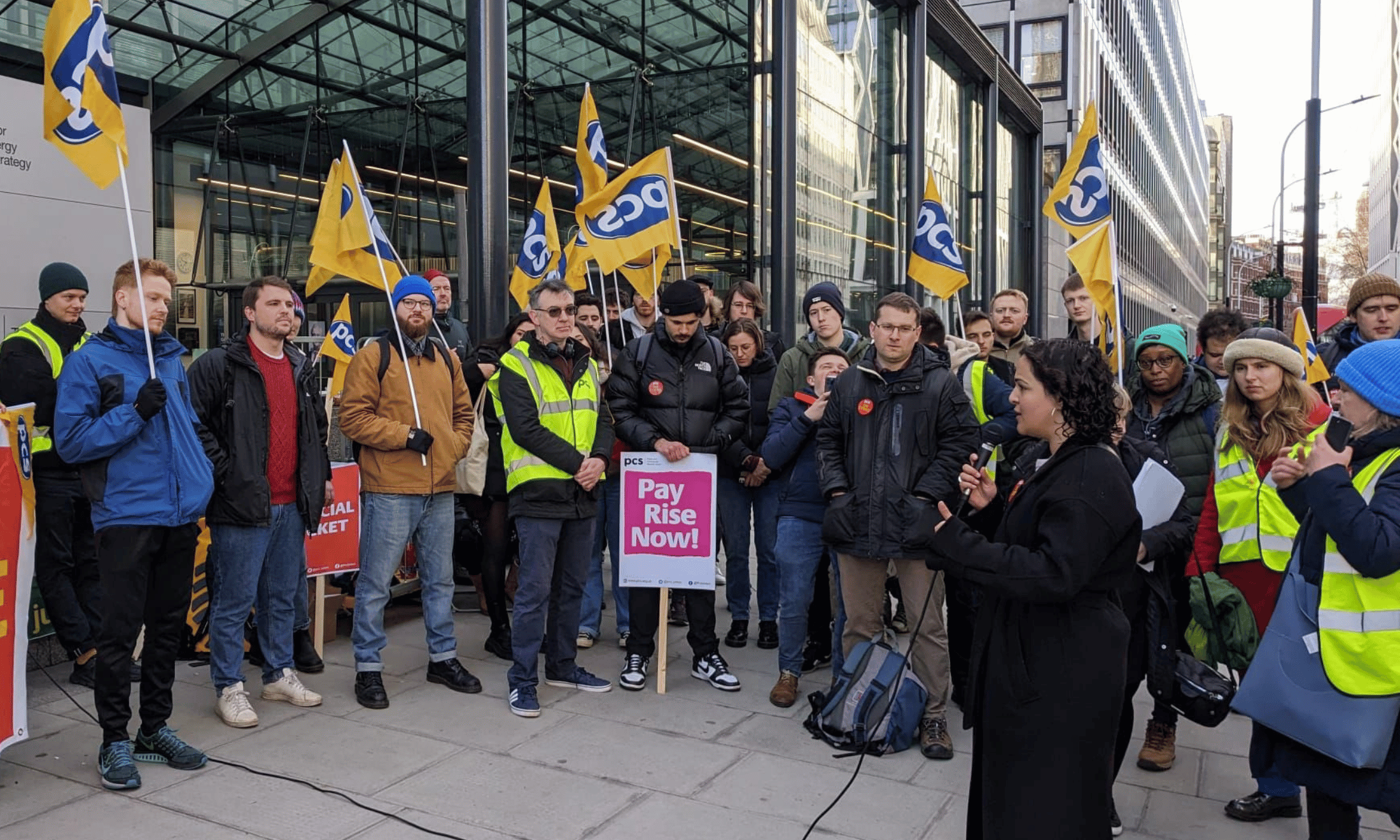
NHS employees are the only health workers in the world who are legally mandated to enact counterterrorism policy as part of their job. Since 2015, the government’s Prevent strategy has required frontline staff across health, social care and education to have “due regard to the need to prevent people from being drawn into terrorism”, with over 7,000 referrals in the first year alone – two-thirds due to fears about Islamic extremism.
Given the reliance on flawed individual judgement, which is subject to unconscious bias, health workers themselves have criticised Prevent training as disproportionately focused on Islam, and carrying the risk of perpetuating racial stereotypes. It is no wonder then, that Muslims are eight times more likely than non-Muslims to be referred.
Through the lens of suspicion, Prevent turns the therapeutic space, which should be a place of safety, into a manifestation of some of the worst fears that people accessing these spaces harbour – the fear of being watched, followed and targeted. I have witnessed firsthand how quickly mention of Prevent or counter-extremism can shut down conversations and cause people to draw into themselves, and studies show that the existence of this duty is a decisive factor in Muslims avoiding mental health services.
“Through the lens of suspicion, Prevent turns the therapeutic space into a manifestation of some of the worst fears that people accessing these spaces harbour – being watched, followed and targeted”
So far, within the NHS, patients have been referred to Prevent for going on Hajj, watching an Arabic YouTube video, and for simply being a refugee from the Middle East. Structural racism and Islamophobia already underlie significant gaps in accessing mental healthcare. Minoritised communities are 40% more likely to access mental health services through the criminal justice system than white people. Meanwhile, fears of personal information being passed by NHS workers to the Home Office deter 50-60% of migrants of African, Caribbean and Asian backgrounds from accessing healthcare.
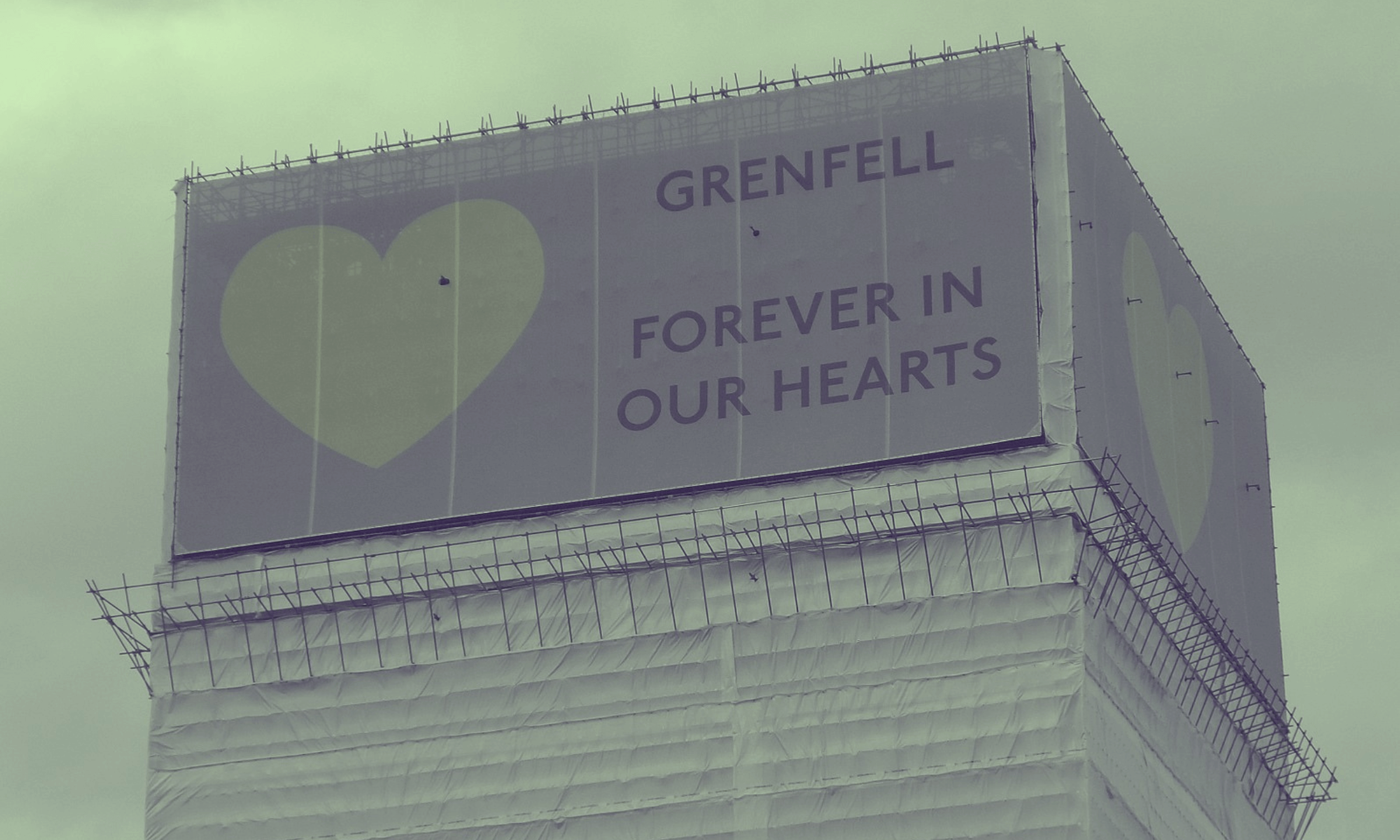
As a mental health professional working in the NHS, it is my job to provide care for people at some of the most vulnerable points of their life. My patients are often living in violent social circumstances, many of them have been traumatised by poverty, state neglect and isolation as their neighbourhoods are gentrified and their loved ones driven out. Their communities are policed and many are subject to state violence that continues to be experienced in various forms when they receive healthcare, such as being refused life-saving cancer treatments on the basis of migration status.
Many of the factors identified as influencing someone’s vulnerability to extremism, such as family tensions, peer pressure, lack of self-esteem and personal and political grievances, are found in those seeking care in a typical psychiatric clinic. So many of the people I see feel angry, upset, threatened, isolated and abandoned by society. They desire purpose and a sense of belonging. When almost every patient presents like this, health workers end up relying on racial signifiers, indices of ‘Muslimness’, to inform their judgement of who might go on to be a terrorist. A white patient struggling to pay their energy bills, who repeatedly tells me in clinic that “the Tories are scum who deserve a taste of their own medicine”, is unlikely to be seen as condoning violence, whereas the Muslim teenage boy who is outraged by the occupation of Palestine is less likely to be afforded the same benefit of the doubt.
“Psychiatry and psychology have a dark history of being subverted and co-opted to medicalise and ultimately depoliticise suffering”
Even if the Prevent referral amounts to nothing, the experience of being approached by a police officer or subject to investigation is terrifying, and for some can be enough to destroy all trust in health services long term. And after all this, there is a lack of available evidence that Prevent actually protects the public from terrorism.
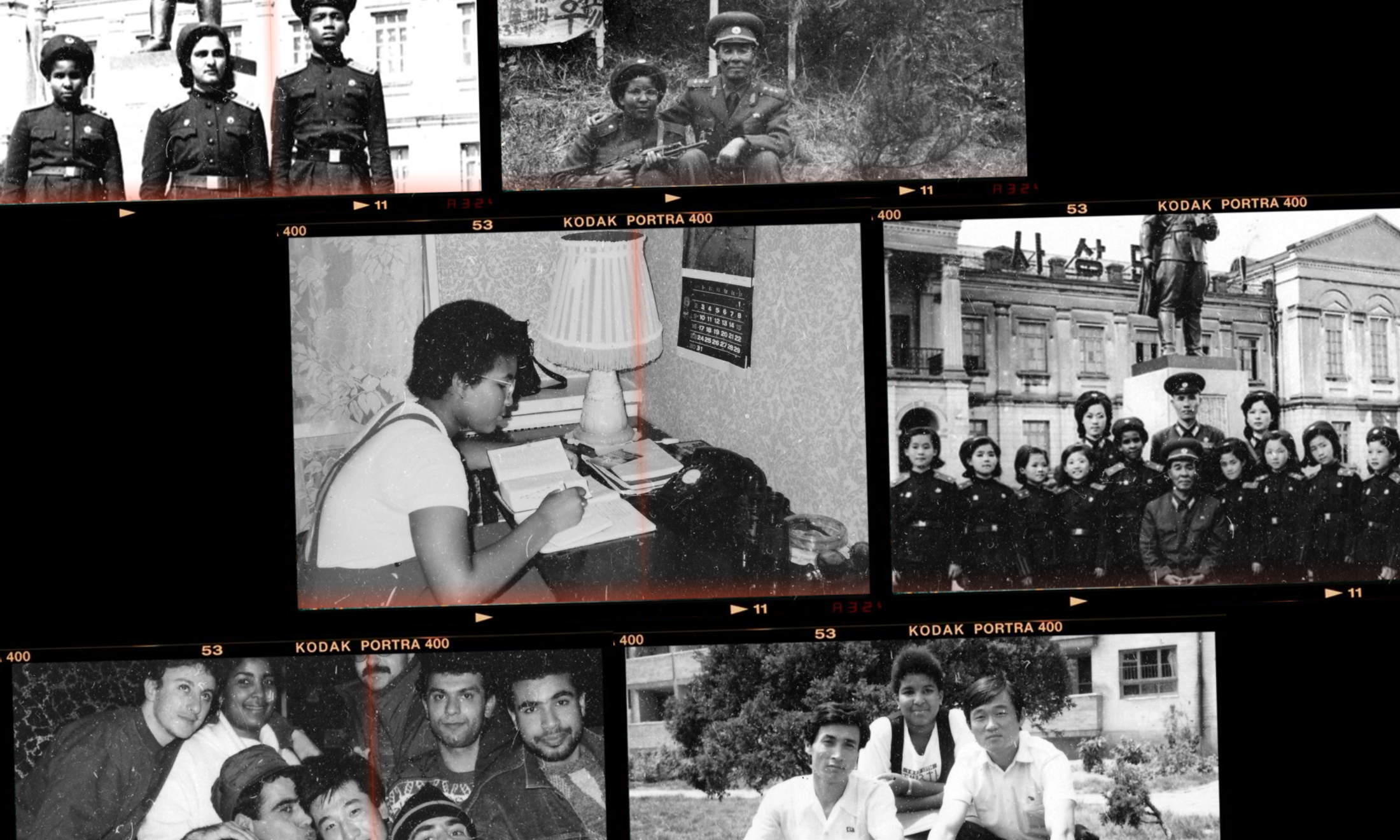
Psychiatry and psychology have a dark history of being subverted and co-opted to medicalise and ultimately depoliticise suffering, severing the link between structural oppression and its health and social consequences on marginalised groups. The violent potential of psychoanalysis steeped in racist and colonial knowledge structures is something that revolutionary and psychiatrist, Franz Fanon, warned against decades ago. As he wrote in Black Skin, White Masks, “the white gaze, the only valid one, is already dissecting me. I am fixed”.
The Prevent scheme follows on from this past, and has been accused by human rights organisations of being Islamophobic, discriminatory and of limiting freedom of speech, confirmed by the People’s Review this year. Yet leaks from the Shawcross review of Prevent in May suggested the programme should crackdown even further on Islamic extremism.
This would make equitable mental health care for minorities impossible. As a concerned clinician, but also as a Muslim myself, I believe that Prevent criminalises Muslim mental distress and should have no role in healthcare or in society.
I don’t want my Muslim patients to be scared of going to see their GP or their NHS therapist, for fear that their words and actions may be perceived as sinister or indicative of a “pre-criminal” state of mind. They should be able to speak openly about what they are experiencing and feel safe in the therapeutic space as we work together with empathy and an open mind.
Mashal is a member of MedAct, a Global Health charity which campaigns against the Prevent duty in healthcare.
Our groundbreaking journalism relies on the crucial support of a community of gal-dem members. We would not be able to continue to hold truth to power in this industry without them, and you can support us from £5 per month – less than a weekly coffee.
Our members get exclusive access to events, discounts from independent brands, newsletters from our editors, quarterly gifts, print magazines, and so much more!