Decolonising Healthcare: we cannot be complacent about black women and HIV
Annabel Sowemimo
05 Dec 2018
Image via Nothing Without Us
The HIV/AIDS epidemic is a perfect example of how sexual and reproductive health remains colonised, yet we have come far in our fight for adequate access to antiretroviral treatment (ART). At the start of the epidemic in the 1980s, the growing number of people in sub-Saharan Africa dying from a mysterious new illness, then known as “Slim”, was widely ignored by both the media and policymakers. In post-apartheid South Africa where black South Africans were understandably wary of accepting Western assistance, the virus quickly spread and killed millions. Groups like the Treatment Action Campaign pushed hard for open access to life-saving ART.
In the week following World Aids Day, it should feel like we have something to celebrate: we now know that those on ART with an undetectable viral load cannot transmit HIV, and will have a normal life expectancy. UNAIDS set ambitious “90-90-90” targets to be met by 2020. They want 90% of all people living with HIV to know their HIV status, 90% of all people with diagnosed HIV infection to receive sustained antiretroviral therapy and 90% of all people receiving antiretroviral therapy to have viral suppression. Botswana, Cambodia, Denmark, the Netherlands, Namibia and now the UK have already been successful in meeting these targets yet, in several areas we continue to struggle.
In 2016, it was found that 79% of women accessing HIV care in the UK were from BAME backgrounds. Migration from regions with high rates of HIV is a factor in this high rate, but intimate partner violence, Female Genital Mutilation (FGM) and socio-economic disadvantage work to heighten the risk of black women acquiring HIV. Many of the structural issues that are driving the HIV epidemic are simply not being addressed.
Despite, knowing that pre-exposure prophylaxis (PrEP) can prevent those at highest risk of contracting HIV from acquiring the virus, in the UK there is still no long-term strategy for providing this medication on the NHS. Helping to plug the gap is Prepster, a UK-based charity raising awareness about the barriers people of colour face in accessing PrEP.
Josina Calliste, the strategic lead at Prepster for women, states the barriers women face are unique. “One the big barriers is that black African women prefer to go to their GPs for their sexual health and other medical issues so attendance at sexual health clinics is much lower and that may mean we may need to think of introducing PrEP via GP surgeries – this could take a long time to upscale,” she said. “For women generally, there is a lack of awareness about PrEP as an option and even if they were to go to a clinic and ask for PrEP it may not be provided. They may not be seen by doctors as being in need of PrEP.”
In sub-Saharan Africa, three in four new infections are among girls aged 15-19 years and young women aged 15-24 years are twice as likely to be living with HIV than men. There is an increasing issue with young women engaging in unsafe sex with so-called “blessers” – older men who help pay tuition fees and rent which, is helping fuel the epidemic across the region.
For young people that do contract HIV in these situations, the path ahead is often filled with many challenges. “Young teenage girls find out about their status most of the time after they’ve gotten pregnant. So they have to deal with the realisation that they are pregnant, they are HIV-positive, and that they now have to stick to this lifelong treatment every day – it’s often too much for them,” said Khanyisile Mavimbela, a HIV positive mentor working with mothers2mothers in Swaziland, the country with the highest HIV prevalence in the world.
Globally, the continued oppression of the LGBTQI community continues to drive the epidemic with individuals fearing for their lives and being unable to access care. Amnesty International now lists 33 countries in which homosexuality is illegal. Many of these countries, like Uganda, are implementing archaic laws that stem from colonial rule. In the US, we see how the rights that were so strongly fought for are being challenged and how easy it is for things to regress such as
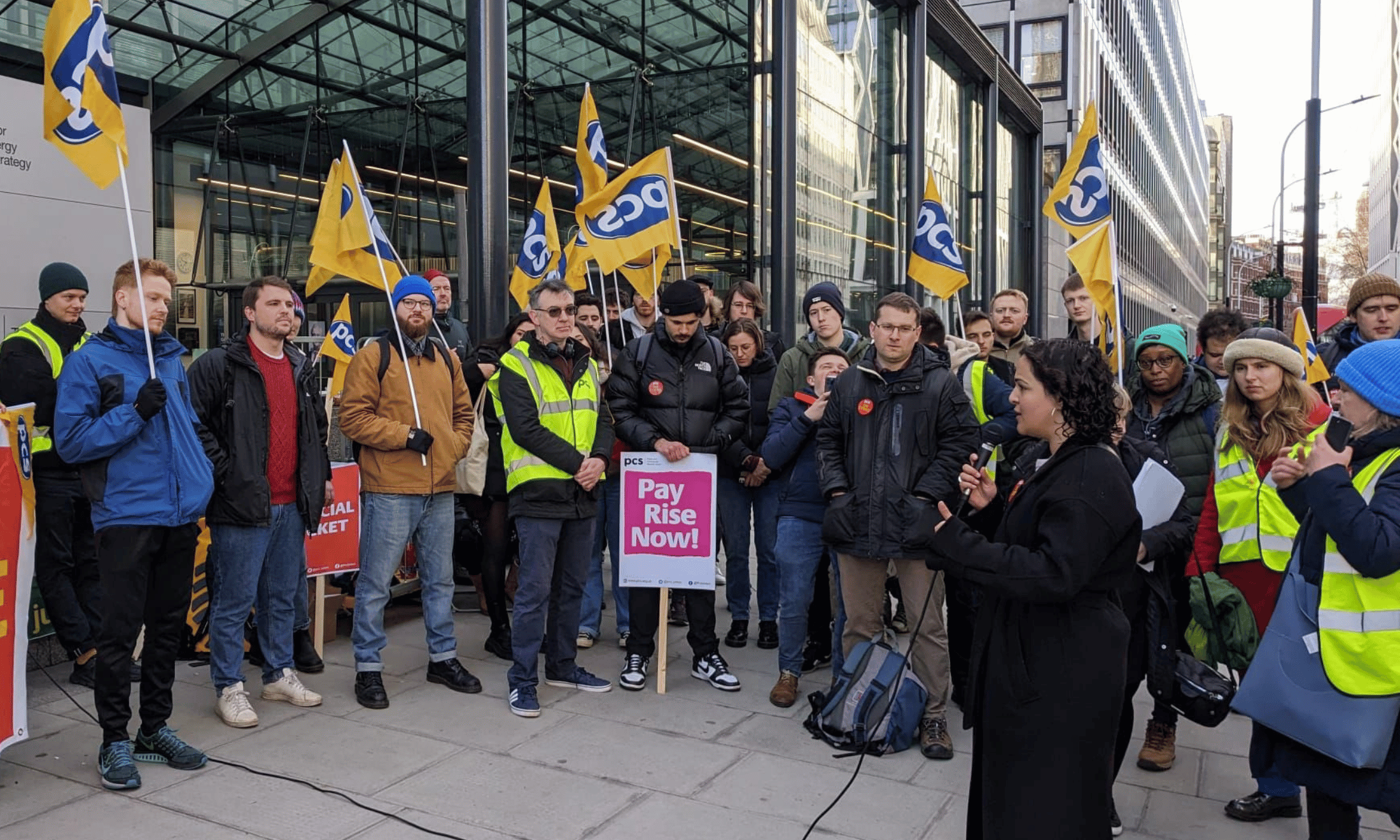
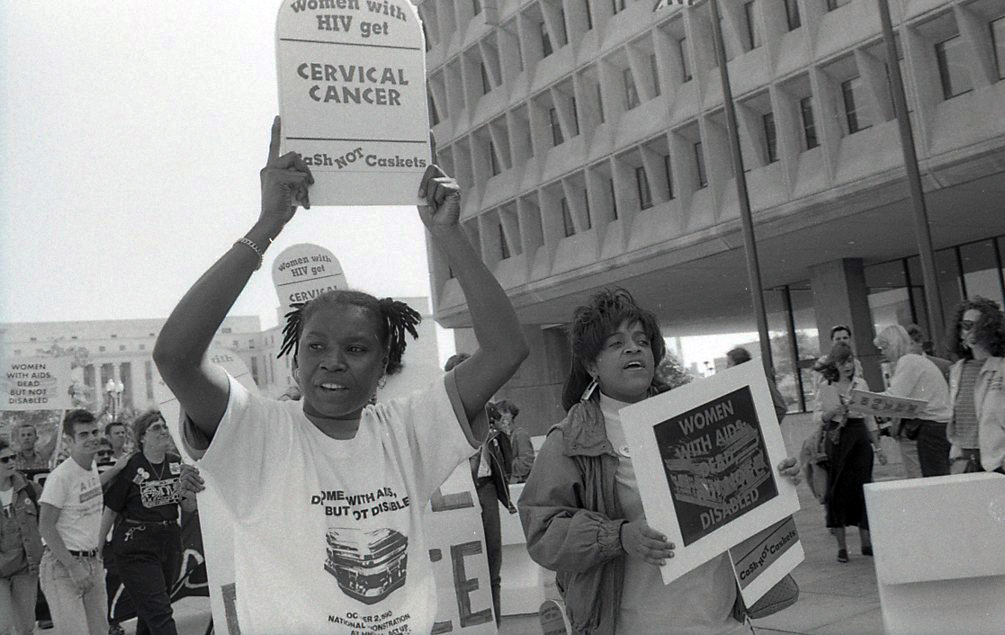
With so much work still to do in addressing the large health disparities within the HIV epidemic, it was uplifting to attend an event this week hosted by Black Femme Film and NAZ Charity film screening of Nothing Without US – a film that chronicles the lives of predominately black women activists who fought to be recognised as individuals living with AIDS (known then as GRID – gay related immunodeficiency disease). At that time “women did not simply have AIDS, they died of AIDS”.
Although we have made huge strides in tackling HIV, the statistics continue to show us that many are still dying of AIDS in huge numbers. When it comes to black women in particular, there is no room for complacency.
For more information about the above or support about HIV and AIDS please visit:
NAZ Charity – UK based charity focusing on sexual health in BAME Communities
Body & Soul – A UK based charity providing support to young people living with HIV
mothers2mothers –an international NGO founded in Cape Town, South Africa in 2001. m2m employs and trains HIV-positive women to deliver health services, advice, and support to women and their families at health facilities and in local communities
Terrence Higgins Trust – A UK based charity which continues to be instrumental in the campaigning against HIV
Prepster’s #PrEP4women – a UK based charity educating and agitating for PrEP as a tool for women’s sexual wellbeing

Britain’s policing was built on racism. Abolition is unavoidable
How Pakistan’s Khwaja Sira and transgender communities are fearing and fighting for their futures

Their anti-rape performance went viral globally. Now what?