Canva/unDraw
Why healthcare workers need us to stop framing the NHS as a racial utopia
The UK's national health service was founded on principles of equality but evidence suggests systemic racism is blighting the careers of Black and brown employees.
Priyankaa Joshi
10 Feb 2021
“Coming from the private sector, I saw the NHS as this mystical place free from the racism and discrimination you experience elsewhere,” says Leena*. The 29-year-old clinical trials practitioner started working for a London NHS hospital in 2018, after her three-year stint at a privately-owned pharmaceutical company. “I moved to the NHS because, based on its ethos, I thought it would be fairer in terms of equal opportunities and career progression,” she explains.
But Leena, who is of Afro-Caribbean and South Asian heritage, quickly had a reality check. “I realised having lots of Black and brown faces in the workforce doesn’t mean anything if everyone in a position of power is white,” she says. “From the get-go, my colleagues made assumptions about me and my abilities based on my race.”
Leena recalls a particular incident during a progress review when her manager said she finds it hard to give Leena criticism because she is scared of how she’ll react. “She barely knew me and I had never shown any anger but she was tarnishing me with the ‘angry Black woman’ stereotype.”
“I was shocked,” she continues. “I think this sort of racial stereotyping has affected my progress and to be honest, it’s really upsetting.”
The NHS is the UK’s largest employer of Black and brown people, with 19.7% of staff coming from a “BAME” (Black, Asian and minority ethnic) background. Founded in 1948 on the principles of social justice and fairness, it’s often lauded as a site where people of colour can realise their potential.
The NHS Constitution includes a duty “not to discriminate against patients or staff and to adhere to equal opportunities and equality and human rights legislation”. Yet, despite having one of the most ethnically diverse workforces in the public sector, evidence shows the health service is failing people of colour in its workforce. And for Black and brown women, who face discrimination based on their race and gender, things are particularly difficult.
“The NHS is the UK’s largest employer of Black and brown people, with 19.7% of staff coming from a ‘BAME’ (Black, Asian and minority ethnic) background”
Leicester-based hospital director Natasha Garraway-Charles, 46, had high hopes about working in the NHS when she finished her training in 2001. “At nursing college, you get all this talk about equal opportunities so I was really excited about starting my career,” she says.
“It was only when I got into the workplace and there was knockback after knockback that I realised the NHS is no different to any other organisation,” she continues.
Senior jobs in the NHS are, unsurprisingly, dominated by white men. According to the latest Workforce Race Equality Standard (WRES) report, BAME staff are over-represented in lower pay bands and seriously under-represented at higher grades, with just 6.5% at very senior level. People from BAME backgrounds make up just 8.4% of NHS trust board members, who are responsible for overall leadership, ensuring accountability and shaping a healthy organisational culture.
Ethnic minority staff are far more likely to experience bullying, harassment or abuse, less likely to be shortlisted for a job and promoted, and Black and brown doctors are twice as likely to be referred to the General Medical Council – the regulatory body for doctors – for disciplinary action than white doctors.
Despite steps such as the WRES, which was introduced in 2015 to ensure “employees from BAME backgrounds have equal access to career opportunities and receive fair treatment in the workplace”, there has been little progress. In fact, the 2019 NHS Staff Survey found that the percentage of ethnic minority staff who believe their workplace provides equal opportunities for career progression and promotion has fallen from 73.4% in 2016 to 69.9% in 2019.
The brown ceiling
“I feel like I’ve reached my glass ceiling,” says 30-year-old medical secretary Patrice* from Leeds. “I’m at a stage in my career where I want to progress but it’s just not going to happen for me.”
“It’s not what you know in the NHS, it’s who you know. The managers will hire their friends, cousins and godchildren,” she says. “There are no people of colour in senior positions at my hospital. Apart from me, all of the other Black people are cleaners or nurses.”
Patrice feels frustrated she isn’t afforded the same opportunities as her white counterparts. “If you say to management you want to do a course or go for a promotion, they will try and talk you out of it and tell you you’re not ready. But if a white colleague, who hasn’t been in the position as long as you, says the same thing, they’ll be fully supported,” she alleges.
Because of this, Patrice has decided to leave the NHS once the pandemic is over. “We’ll see how the recession pans out but I’m definitely looking to leave because there’s just no career progression for people like me.”
“I left the City to come to the NHS because I thought things would be better but I feel like I need to go back to the City if I want to progress and make money.”
Leena also cites the “cliquey” and “exclusive” culture as one of the reasons she feels stuck. “It’s not about merit or skillset, it’s about who you have lunch with and if you fit in,” she says.
“I know several talented Black people who have gone for job after job but haven’t moved up”
“Because of the colour of my skin and my social background, I feel like I have to work ten times harder than my white colleagues.”
Recently, a promotion opportunity came up in Leena’s team but she was overlooked and the job went to a white woman with less experience. There is no evidence racism was involved in the decision but Leena can’t shake the feeling that there may be discrimination at play. “I asked my manager why I didn’t get the job but she couldn’t give me a valid reason,” she says.
“I am actively trying to leave at the moment because I’m sick of it. I care about my patients so much but the environment is draining,” she tells gal-dem. “I’m done with putting in effort and getting nowhere. I’d rather go elsewhere and hope for better treatment.”
Tough at the top
Unlike Patrice and Leena, Natasha did manage to rise through NHS ranks. After taking the ‘Ready Now’ leadership development programme, an initiative designed to elevate underrepresented groups into NHS management roles, Natasha moved up two pay bands and became a group services manager. However, she admits her experiences aren’t the norm for Black women.
“I was very fortunate to cross paths with some senior non-BAME people who supported my progress,” she says. “I know several Black people with plenty of experience who have gone for job after job but haven’t moved up at all.”
Despite her initial success, Natasha was only able to progress to a certain level, despite watching white colleagues move into more senior positions. Consequently, she left the NHS in 2020 and is now working at a private hospital.
“I was more qualified than most of the people who managed me and seeing other people get jobs they’re not competent to do was extremely distressing,” she explains. “I never thought I’d work in the private sector and it’s sad because my values are aligned with the NHS. But I had to leave because my mental health was being impacted.”
“The number of ‘BAME’ staff who have died in England is seven times higher than white workers”
Discrimination in the health service is nothing new but the pandemic has shone a stark light on existing disparities caused by institutional racism. Analysis by ITV News found that the number of BAME staff who have died in England is seven times higher than white workers.
This is, in part, because Black and brown people are concentrated in lower-level jobs on general wards where there might be less PPE provision and as such are more likely to be exposed to the virus. But a recent report by the NHS Confederation BME Leadership Network shows that discrimination has also been a major factor.
The research revealed that ethnic minority healthcare workers were more likely to take on high-risk roles due to fear that their shifts might be reduced, particularly if they had vulnerable immigration status. Despite the NHS anti-bullying policies, 88% of survey participants said they do not speak up about concerns for fear of losing their jobs.
Leena confirms this. “You could never bring up anything about racism or discrimination. You’d be seen as the trouble-maker and I would be scared of the consequences,” she says.
Lip service
It’s brutally clear that racism and discrimination within NHS culture require urgent attention, but what is actually being done about it?
In March 2020, NHS England set itself a target of 19% representation of ethnic minority employees at every level by 2025. And in May, the NHS Race and Health Observatory, an independent centre hosted by the NHS Confederation, was launched to drive improvement on race equality.
“We know that having a representative and inclusive workforce at all levels will enable NHS workplaces to be best placed to tackle issues and challenges faced by our diverse patients and communities head-on,” Dr Habib Naqvi MBE, director of the Observatory, tells gal-dem. “The Observatory will help support organisations in that regard.”
The latest NHS People Plan, which was published in July, also includes measures to improve the experiences of ethnic minority employees. Yet, according to Suzie Bailey, director of leadership and organisational development at The King’s Fund, without a credible implementation plan, it falls a long way short of the strategy the NHS so desperately needs.
For Patrice, any attempts to improve things so far have been tokenistic. “It’s all lip service,” she says. “After the Black Lives Matter protests, they appointed someone to be in charge of race relations but nothing has come of it. There’s nothing happening to improve diversity as far as I can see.”
“They make it seem like they care about race equality but they don’t,” agrees Leena. “There are only so many unconscious bias workshops you can do and if management is just doing them for the sake of it, nothing’s going to change.”
Reports and reviews aside, until the government and NHS organisations take meaningful action to tackle racial inequalities within the institution and commit to a culture change where people of colour feel valued and supported, women like Patrice, Leena and Natasha will continue to take their skills elsewhere.
*names have been changed to protect identities

Britain’s policing was built on racism. Abolition is unavoidable
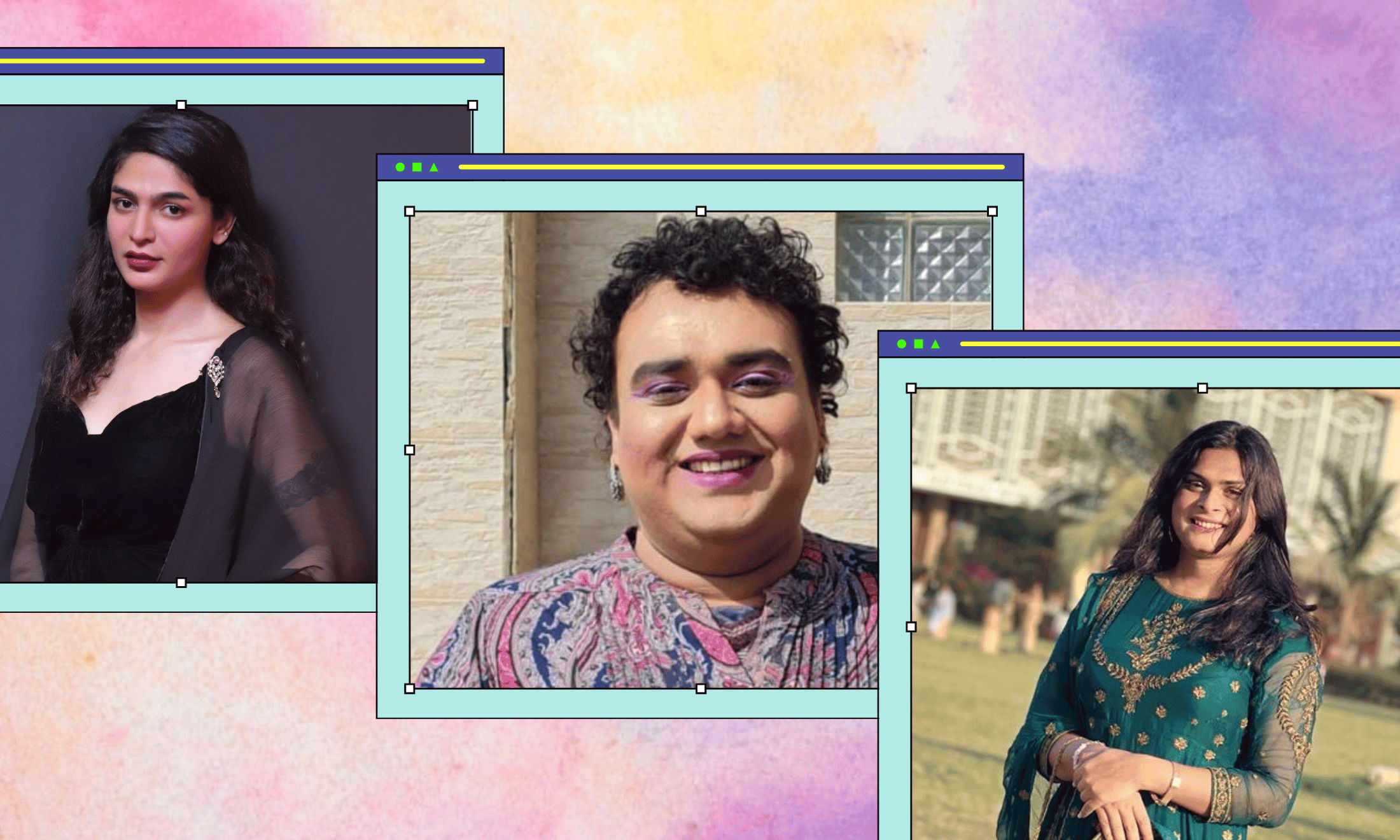
How Pakistan’s Khwaja Sira and transgender communities are fearing and fighting for their futures

Their anti-rape performance went viral globally. Now what?