Tessie Orange Turner
Is fear of medical institutions and professionals killing the Black community?
Iatrophobia should be considered a very real problem in relation to Covid-19 vaccine hesitancy among black people in the UK.
Annabel Sowemimo
26 Jan 2021
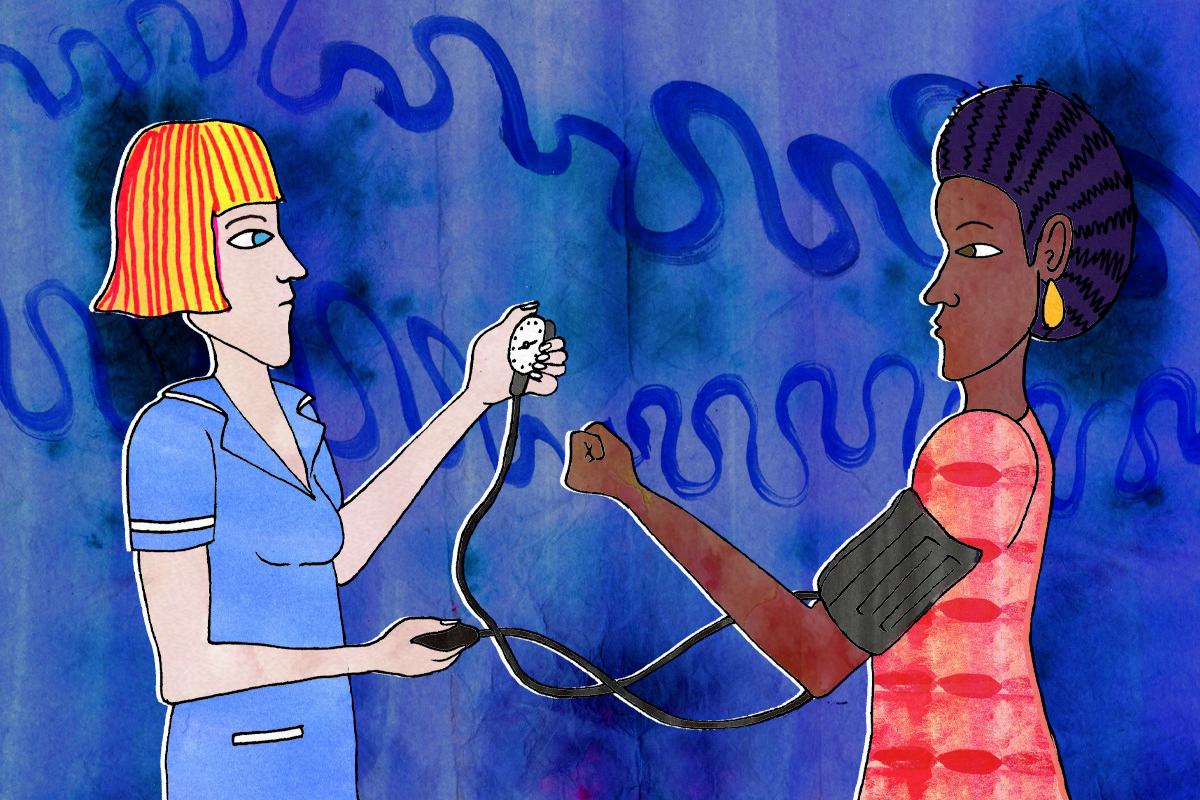
“You don’t look unwell.”
The A&E triage nurse looked me up and down as she took a brief history, eyeballing me and scribbling some notes. I had never felt so atrocious. She rolled her eyes as I muttered that someone should have written a letter. She forcefully applied a blood pressure cuff to my arm and finally shoved a thermometer in my ear – clearly I was upsetting her evening in some way. She let out a slight yelp while showing me the temperature reading. I looked up: 40 (anything above 38 degrees signals likely infection) was flashing on the screen.
“Nigerian – you said? That area is endemic for haemorrhagic fever.” She rapidly backed out of the room, presumably to fetch someone who could put me into isolation. This was pre Ebola and I was left sitting in the room utterly mystified and feeling incredibly ill.
I ended up being admitted for several days and the team on the ward were lovely. I was treated for a severe case of dysentery secondary to shigella flexneri – deeply unpleasant but not haemorrhagic fever. However, the whole experience left me slightly scared. Why had the triage nurse not believed me when I said I felt unwell? Why did she seem to think I was making up the referral letter? If I wasn’t a doctor, emboldened by my own medical education, I would be very reluctant to expose myself to such an unpleasant encounter again. I would have told my friends, family and they too might have retreated from such an encounter.
“If I wasn’t a doctor, emboldened by my own medical education, I would be very reluctant to expose myself to such an unpleasant encounter again”
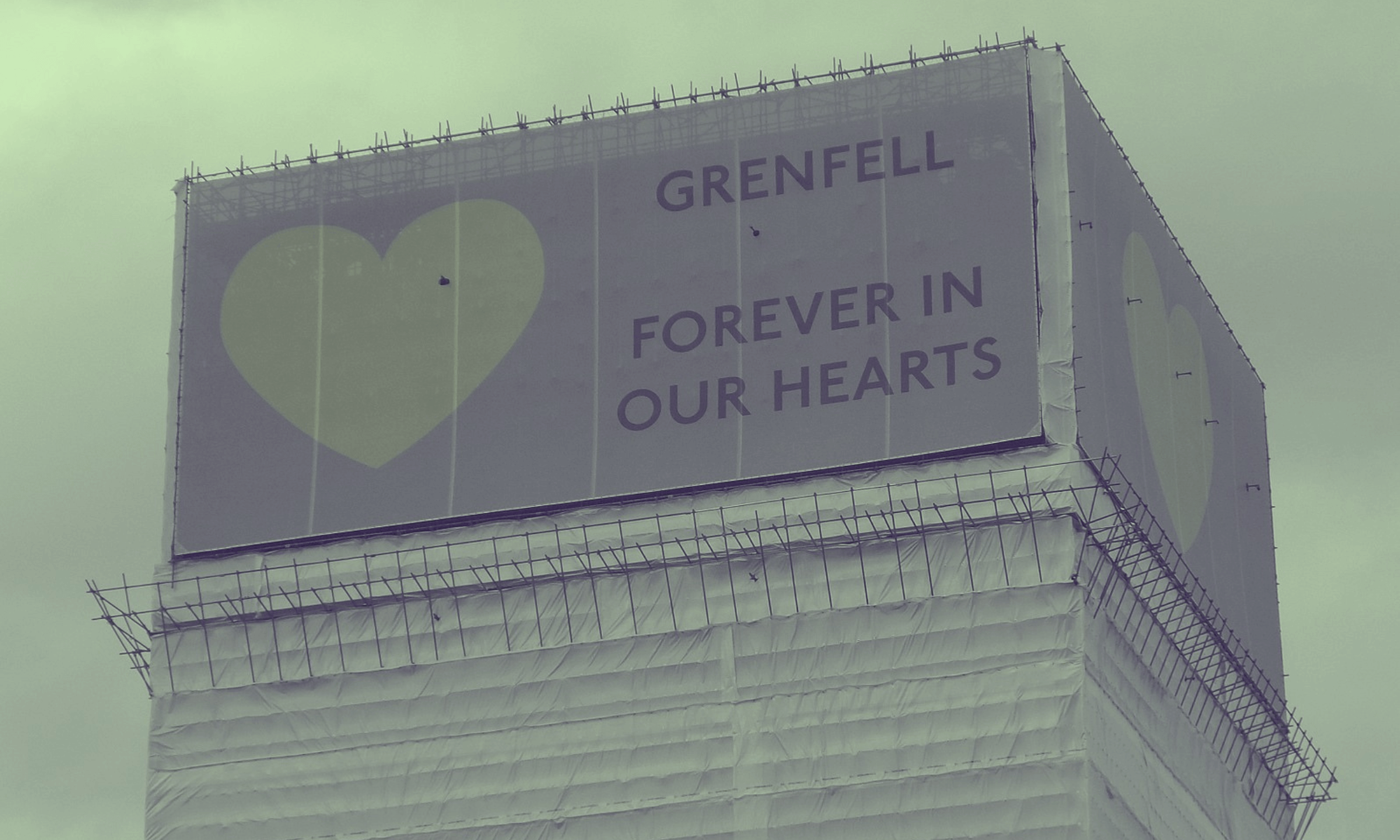
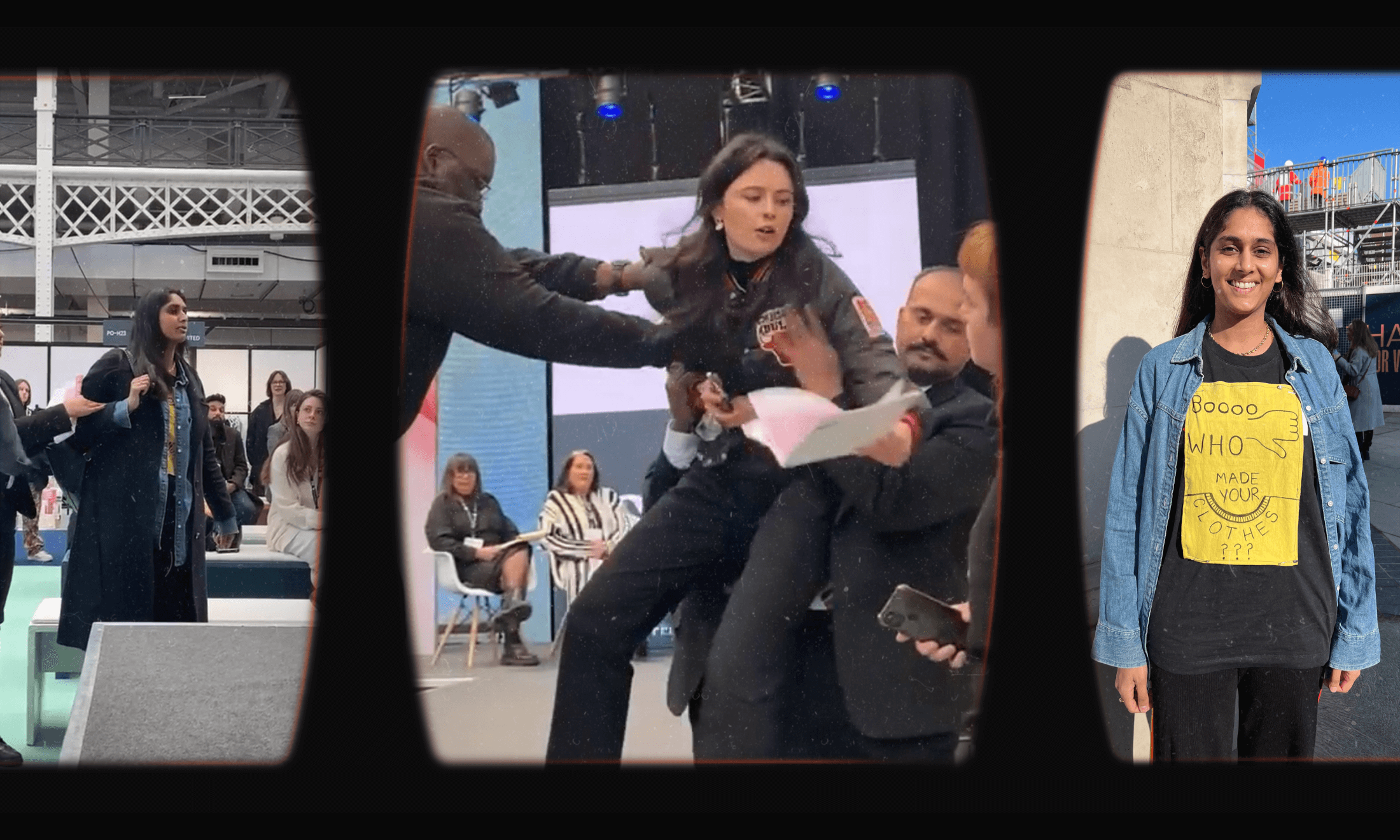
Sadly, this pandemic continues to confirm what many of us have known for some time – my experience was not unique. In the first wave of the pandemic, we learnt about the death of 36-year-old Kayla Williams who died of suspected Covid-19 the day after, being told by ambulance staff that visited her home to administer self-care and that she did not need to go to hospital.
More recently, we saw the videos of Dr Susan Moore, a US-based physician, shared on social media detailing her encounter with medical professionals just days before her death from Covid-19. In the videos, Susan chronicles her days in hospital with Covid-19 and having to fight doctors for medication and treatment – at one point exclaiming: “He made me feel like a drug addict… If I can’t prove I’m in pain then, I can’t get treatment.”
Moore ends on a sober note: “I put forth and I maintain if I was white I wouldn’t have to go through that.” The hospital has launched an urgent investigation into the allegations of racism but for Moore, it’s much too late. Moore’s case, makes many Black people ask if a Black doctor can’t save herself from medical discrimination then, who can?
Author of Medical Apartheid, Harriet Washington was one of the first to use the term iatrophobia; the fear of medical institutions and professionals in relation to the experiences of Black Americans accessing healthcare. In her prize-winning book, she describes the legacy of unethical experimentation on Black Americans and their modern-day experiences with healthcare institutions. As well as these more recent harrowing stories – Black communities regularly cite the colonial history of medical malpractice on their communities from the Tuskegee trials to the failed provision of antiretroviral drugs during the early HIV pandemic.
“I have yet to convince my 86-year-old grandmother to accept the Covid-19 vaccine”
Relatively little research has been done on the experiences of racially minoritised communities and their experiences with healthcare. A recent government report commissioned in the wake of the murder of George Floyd found that 60% of Black people feel that their health is not equally as protected as their white counterparts; this was up to 78% amongst Black women. Yet, we still have no formal steps on how to remedy such statistics amid a global pandemic that continues to disproportionately affect those that are racially minoritised.
Conversely, we see how social media has further reinforced pre-existing mistrust within Black communities towards the healthcare system. The new social media app Clubhouse allows people to have an open discussion with strangers. Earlier this month a Black doctor was allegedly bullied by Chakabars – a man who has become an internet sensation thanks to his eco-lifestyle and anti-science stance – and comedian Tiffany Haddish. As the doctor tried to correct misinformation around the vaccine, Chakabars and Tiffany launched a scathing campaign; stating that such doctors were acting in the interest in white supremacy.
I have yet to convince my 86-year-old grandmother to accept the Covid-19 vaccine – something that weighs heavily on my heart. My dad, a GP working in East London – an area with a historic West Indian community – shared his growing worries as nearly all his Black patients over 80 continue to decline their vaccinations. “The nurses will say – there’s a video of Dr George on the website having his Covid-19 vaccination,” he tells me. “They just look at us like we are all mad.”
Whilst iatrophobia may still be nonsensical to some – unreasonable even, given the wealth of information that many of us now have at our disposal due to social media – it is often driven by logic and history for self-preservation. If a child burns itself on a kettle, they learn not to touch the kettle again.
With a recent household survey revealing that almost 72% of Black or Black British people are unlikely or very unlikely to take the Covid-19 vaccine perhaps it is time to reflect on the legacies that have created this statistic. If a global pandemic which has now claimed over 2 million lives and that of over 91,000 in the UK does not make us question our current practice, then what will?
There remains an urgent need for further research into the attitudes and experiences of racially minoritised groups navigating healthcare systems. The implication of provider bias on health inequalities and a willingness to accept that healthcare is not a neutral playground.