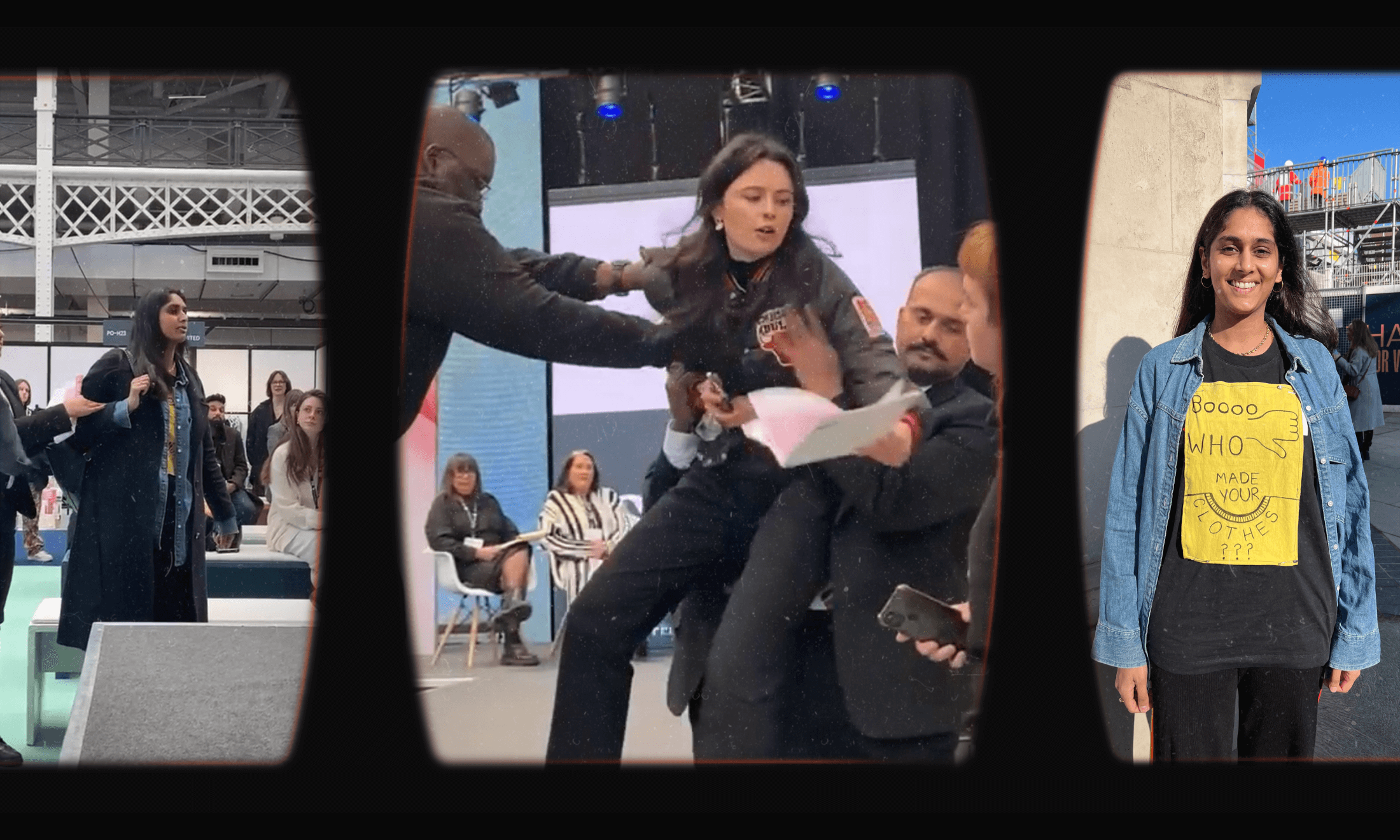
Illustration by Ragavee Balendran
Diagnosis, expected: what I experienced during treatment shows health disparities aren’t as random as we think
From pale pink prosthetic breasts to forgotten pain relief post-surgery, Tashmia Owen details how her cancer treatment in hospitals echoes many who fall through the cracks.
Tashmia Owen
02 May 2020
Illustration by Ragavee Balendran
Microaggressions, white feminist tears, workplace bullying, dating, the school gate drop off, beauty halls, tone policing, hosiery, lingerie, plasters. The relentless, insidious way our every day reminds us as black and brown women that we are not accepted as the norm, not seen as belonging. As being of any relevance to the global experience.
There is a social patterning in the inequalities we face, entrenched in the systems around us, like bumpers in a fairground, bouncing us back to the direction we are meant to keep, to the lives we have permission to live. When life feels as though it is spiralling, there is the guiding hand taking us back, to the places we have been designated to reside in. Those who hold the power are looking after us.
I had my first mammogram in July 2016, the doctors stated it was all clear, there was nothing of concern, my history and demographic made it highly unlikely and I was sent home being told they will see me in a year. I did not hear from them again. Having treatment for complex post-traumatic stress disorder (CPTSD) most of my symptoms were regularly attributed to that. Trauma playing out in my body, psychosomatic symptoms.
In January 2019, I had my second mammogram. The doctor performing the ultrasound was a South Asian man of a similar age to me. He looked me in the eye saying the pain you describe is not something I want to leave unexplained. He took a biopsy, a fierce punch in the breast, the memory of it sits on my skin today like a shadow. I left the hospital and cried. Relief and sadness for being believed, for being heard, for the way he looked me in the eye and saw me. Three days later I was called to come in immediately. It was cancer, undetectable in mammograms. Late Stage 3, caught just in time, a chance to remove it, to see a few more years of my children’s lives.
“I had laid there for days, with morphine sitting in my bed, that was not dispensing into my veins”
In September, preparing for surgery, a team of medics appeared in the changing room, seven to nine people I had never met before, as I pulled up compression socks in my backless gown. They were the doctors who would be performing my surgery
For 11 months I had planned with two consultants, they had looked at my body, drawn-out where the incisions would be made, built up a relationship with me as I asked about each stage of what they would do to me. Yet here I was listening to a doctor whose face did not match the one I had prepared to see, no explanation given. The words floated around the room as I grappled with being tossed away without any warning. If I did not have dear friends present at these moments I would question my memories of them, having them with me to advocate for me and give me the strength to speak up for myself was critical to everything that happened.
Darkness, ice-cold rods shooting through my body, my jaw attempting to dance away from my skull. The anaesthetist and surgeons face drifting into my eye-line, we have you, it has been a long time, you were under for 12 hours, reconnecting blood flow... I heard as I faded out. Once on the ward, I asked for pain relief, my torso ripping apart, I was up to my limit and had to wait.
This conversation repeated itself in circles, the outcome never changing. A visit from the anaesthetist led to me joking if they would ever, without consent, use placebos as I could not comprehend the level of pain I felt. A friend had to insist on the answers they were not giving me until an oversight with my medical chart was spotted.
I had a device left feeding morphine into my abdomen for three days. On the day a nurse removed it we both looked in horror realising it had not been activated. I had laid there for days, with morphine sitting in my bed, that was not dispensing into my veins. Paracetamol and Ibuprofen after a mastectomy and transplant surgery and not one doctor believed me or checked why I was in pain and so alert immediately after surgery. Recalling those moments I have to close them in on themselves, I cannot look for too long or feel again that sensation of waking up in a snuff movie. It aches to think of a person experiencing this in a hospital, but it is one of many many stories from black and brown women globally.
Visiting the prosthetics department I was overwhelmed by the lack of awareness as I was told to choose from a lineup of pale pink breasts. My goldfish-like response irritated the woman dealing with me as I tried to explain how I was not used to shopping for a breast let alone one from another race.
“Visiting the prosthetics department I was overwhelmed by the lack of awareness as I was told to choose from a lineup of pale pink breasts”
I questioned the percentage of South Asian women who got cancer. There was little visibility, on national campaigns, in documentaries, on TV. The repeated questions from every specialist about my family history – why could I not find out my relatives medical history? The pain, embarrassment and frustration I felt as I repeatedly explained how medical information was not collated that way historically in Bangladesh. Some families did not dwell on the reason for a person’s death or speak about illnesses that were connected to people with anatomy like mine. It was private, a taboo, almost as though it did not exist.
The look of confusion and inability to understand by medical staff ensured my interpretation that it was not something they had ever encountered. I could not explain how on top of the fear I felt – the guilt that I was not going to be around to parent the people I had brought into this world – I could not face the blame for having contracted this disease in the first place. I could not bear to hear the words you have not followed Allah’s path and led a righteous life, what did you think would happen? The act of searching out certain people held harm and pain for me.
From the early stems of my treatment through the unfurling of each stage I had to fight to have my voice heard.
Each time I experience this cognitive dissonance I feel as though a huge force has slammed me against the wall. My breathing becomes shallow, an inability to walk away occurs despite it being the only thing I want to do. My thoughts and words wiped away in my presence, as they leave my mouth, grappling to hold onto each breath as the recipient extinguishes them, denying I had exhaled. However many times I experience this act of violence I have not developed an ability to protect myself. I become a hostage in a situation I am fighting to gain control in.
In waiting rooms, sometimes I receive a frustrated sigh if I mention my name is said just as it is written. Weeks ago, I sat in a room with one other patient, a Polish woman, who had her hand shook and was told by the doctor she was really happy to meet her. I prepared for the same welcome to only be asked abruptly and loudly, “but what are you here for? Who is your appointment with?” She was the only person in the department; all other appointments were postponed due to Covid-19. She was not happy to meet me.
“In waiting rooms, sometimes I receive a frustrated sigh if I mention my name is said just as it is written”
The moments are endless, the reasoning relentless, paranoia, seeing opposition and strife when it is not present. One day while receiving chemotherapy, a patient – a white man – arrived and sat in the chair beside mine. I smiled and greeted him as he prepared to have his treatment. As the nurse inserted a cannula into his arm I glanced over, his skin a sleeve of ink. Drifting in my thoughts a realisation jerked me back to his arm, swastikas among the sea of colour. My eyes met that of the nurse, a Nigerian woman with patience I have yet to see matched. Both of us silently knowing the strength it takes to remain, the toll it takes every day your existence is shown to be disposable, despised, solely there as a commodity for others.
Once I found myself in the hilarious and uncomfortable position of having my history taken by an Indian man medic who could not meet my eyes. Each time he uttered the word breast he addressed my knees, a few times he asked about my menstrual cycle, the agony of it all led him to asking my breast directly….
It is in our health systems, so deeply ingrained in the belief of our strength, stoicism, our existence not registering as those that require retaining. The assumption that we prefer certain ways of living, so carefully guided back should we be confused and stray. Black women lose their lives disproportionately to any other woman in childbirth, yet we do not hear the deafening voices. Like so many conversations their lives are erased, as though they were never lived, never loved.
When a simple plaster comes in one shade fits all nude, the message is clear. The white experience is the defining norm, it holds the power, and informs us all what is to follow, and who will survive.
This part of Tashmia’s Diagnosis, expected series